
Proton Therapy for Prostate Cancer: Effectiveness, Benefits, and Clinical Evidence
Proton therapy has emerged as a promising treatment modality for prostate cancer, offering potential advantages over traditional radiation therapy techniques. This advanced form of radiation therapy uses protons instead of photons to target cancerous cells, allowing for more precise dose delivery while minimizing exposure to surrounding healthy tissue. As prostate cancer remains one of the most common malignancies in men, understanding the efficacy and safety profile of proton therapy is crucial for patients and healthcare providers making treatment decisions.
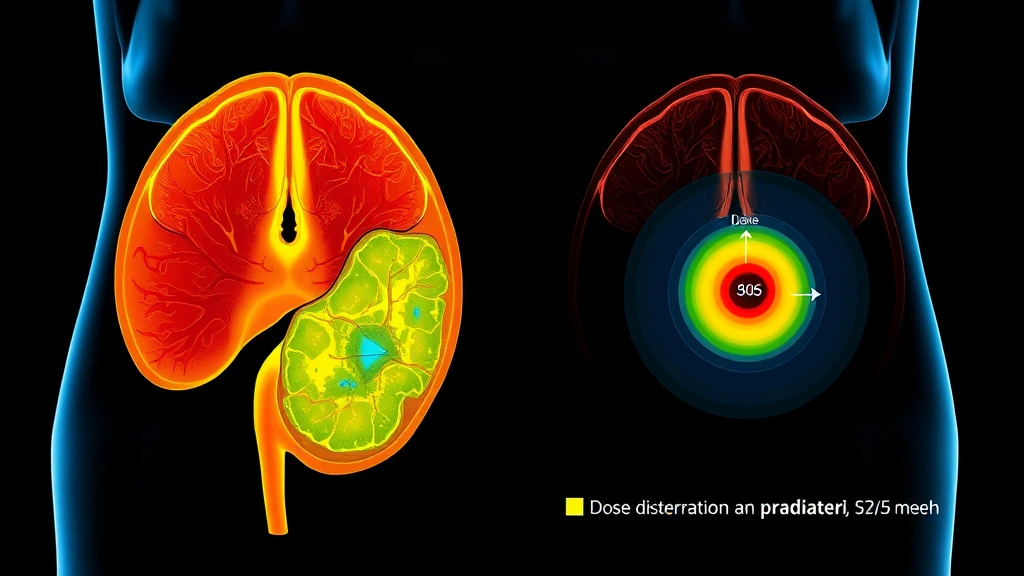
The fundamental difference between proton therapy and conventional external beam radiation therapy lies in how energy is deposited in tissue. Protons release most of their energy at the end of their trajectory, creating what physicists call the Bragg peak. This characteristic allows clinicians to concentrate therapeutic radiation directly on the tumor while sparing adjacent organs such as the bladder and rectum, potentially reducing long-term side effects that can significantly impact quality of life.
Understanding Proton Therapy Technology
Proton therapy represents a significant advancement in radiation oncology, utilizing charged particles rather than photons to treat cancer. The technology works by accelerating protons to approximately 70% the speed of light before directing them toward tumors. Unlike photon-based radiation, which deposits energy gradually throughout its path and continues beyond the target, protons deposit minimal energy at the entry point and maximum energy at the Bragg peak—a narrow zone where the proton comes to rest.
The precision of proton therapy is particularly valuable in treating prostate cancer because the prostate gland is surrounded by critical structures including the rectum, bladder, and penile tissues. By concentrating the therapeutic dose precisely on the prostate while minimizing dose to surrounding organs, proton therapy theoretically reduces the risk of treatment-related complications. Modern proton therapy systems employ intensity-modulated proton therapy (IMPT), which allows clinicians to modulate the beam intensity at different depths, further optimizing dose distribution.
The clinical implementation of proton therapy requires sophisticated treatment planning. Radiation oncologists and medical physicists use advanced imaging, including CT and MRI scans, to delineate the prostate and nearby organs at risk. Treatment planning systems calculate the optimal proton beam arrangement and energy levels to deliver the prescribed dose to the tumor while respecting dose constraints for normal tissues. This meticulous planning process distinguishes proton therapy from simpler radiation approaches.
Clinical Efficacy in Prostate Cancer Treatment
Research published in leading oncology journals has demonstrated that proton therapy achieves excellent tumor control rates in prostate cancer patients. A landmark study from the National Institutes of Health examining proton therapy outcomes showed five-year biochemical recurrence-free survival rates exceeding 90% in patients with low to intermediate-risk disease, comparable to or better than outcomes with conventional photon-based radiation therapy.
Intermediate and high-risk prostate cancer patients also benefit from proton therapy, particularly when combined with androgen deprivation therapy. Clinical trials have shown that proton therapy delivers effective tumor control with favorable toxicity profiles compared to conventional external beam radiation therapy. The ability to spare surrounding tissues while maintaining therapeutic efficacy makes proton therapy an attractive option for many patients.
Long-term follow-up data continues to accumulate, with some centers reporting 10-year biochemical control rates above 85% for low-risk patients treated with proton therapy alone. These results support proton therapy as a legitimate treatment option comparable to or superior to conventional approaches. However, it’s important to note that treatment success depends on multiple factors including patient age, comorbidities, disease stage, and adherence to treatment protocols.
For patients considering rehabilitation and recovery support following proton therapy, understanding the typical recovery timeline is essential. Most patients experience minimal acute side effects during treatment, with recovery progressing rapidly after completing the course of therapy.
Comparing Proton Therapy to Conventional Radiation
The comparison between proton therapy and conventional intensity-modulated radiation therapy (IMRT) has become increasingly relevant as proton facilities expand. While both modalities achieve excellent tumor control rates, they differ significantly in their dose distribution characteristics. Conventional IMRT uses multiple photon beams to conform radiation to the prostate shape, but photons deposit dose throughout their entire path, including beyond the target.
Proton therapy’s physical advantages include reduced exit dose, meaning tissues beyond the prostate receive substantially less radiation. For a young patient with 40+ years of life expectancy following treatment, this dosimetric advantage may translate to reduced risk of secondary cancers and late toxicities. Conversely, conventional IMRT has decades of follow-up data and is widely available, making it a proven, accessible option.
A comprehensive analysis from the National Cancer Institute indicates that both approaches yield similar biochemical control rates when properly executed. The choice between modalities should consider patient factors, tumor characteristics, institutional expertise, and access to technology. For patients interested in comprehensive cancer care approaches, understanding all available treatment options—including rehabilitation considerations discussed in physical therapy assistant training programs—ensures informed decision-making.
Some controversy exists regarding whether the theoretical dosimetric advantages of proton therapy translate into clinically meaningful reductions in late toxicity. Retrospective studies suggest potential benefits, particularly for younger patients and those with extended life expectancies, but prospective randomized trials are ongoing to definitively answer this question.

Side Effects and Toxicity Profile
Proton therapy generally produces a favorable side effect profile compared to conventional radiation therapy. Acute side effects during treatment typically include urinary frequency, urgency, and dysuria (painful urination), as well as mild rectal symptoms such as diarrhea or urgency. These acute effects are generally manageable and resolve within weeks to months after completing treatment.
The more important consideration involves late toxicity, which develops months to years after treatment completion. Late genitourinary toxicity can include erectile dysfunction, urinary incontinence, and chronic urinary symptoms. Late gastrointestinal toxicity may manifest as rectal bleeding, fecal incontinence, or chronic diarrhea. Proton therapy’s reduced dose to tissues beyond the prostate theoretically minimizes these late effects, though long-term comparative data continue to accumulate.
Grade 3 or higher late toxicity rates with proton therapy are reported in the literature at rates of 5-10% for genitourinary complications and 2-5% for gastrointestinal complications, depending on dose and fractionation schemes used. These rates are generally favorable compared to historical photon therapy data, though direct randomized comparisons are limited. Patient factors such as pre-existing urinary or bowel dysfunction significantly influence toxicity risk regardless of treatment modality.
The impact of toxicity on quality of life should not be underestimated. Erectile dysfunction affects the majority of men treated with any form of radiation therapy for prostate cancer, though the mechanism and timeline of onset may differ between treatment modalities. Patients should have realistic expectations about potential side effects and engage in shared decision-making with their oncology team.
Patient Selection and Candidacy
Not all prostate cancer patients are ideal candidates for proton therapy. Patient selection should consider disease stage, risk stratification, patient age, comorbidities, and life expectancy. Low-risk prostate cancer patients with small, localized tumors and PSA levels below 10 ng/mL represent ideal candidates for proton therapy, as they have excellent long-term survival and minimal risk of metastatic disease.
Intermediate-risk patients with PSA levels between 10-20 ng/mL or Gleason scores between 7 benefit from proton therapy, particularly when combined with short-course androgen deprivation therapy. High-risk patients with extensive disease, high PSA levels, or aggressive histology may require combined-modality therapy including prolonged hormone therapy, and proton therapy can be effectively integrated into these comprehensive treatment plans.
Patients with inflammatory bowel disease, prior pelvic radiation therapy, or severe urinary symptoms at baseline represent relative contraindications for proton therapy, though not absolute ones. These patients require careful evaluation and may benefit from alternative approaches. Understanding the role of rehabilitation professionals, as discussed in occupational therapy programs, can help patients prepare for potential functional impacts of treatment.
Age is an important consideration, with younger patients potentially benefiting more from proton therapy’s reduced late toxicity risk due to their longer remaining lifespan. Men over age 75 with significant comorbidities and limited life expectancy may derive less benefit from proton therapy’s theoretical advantages over conventional radiation.
Cost Considerations and Accessibility
Proton therapy’s higher cost represents a significant barrier to widespread adoption. Treatment costs typically range from $30,000 to $50,000, compared to $15,000 to $25,000 for conventional IMRT. Insurance coverage varies, with some plans requiring prior authorization or limiting proton therapy to specific patient populations. Medicare generally covers proton therapy for prostate cancer, though coverage policies continue to evolve based on emerging evidence.
The limited number of proton therapy facilities worldwide creates geographic accessibility challenges. Many patients must travel considerable distances to access proton therapy, adding burden and expense to treatment. As proton therapy technology advances and becomes more efficient to operate, costs may decrease and accessibility may improve, though this remains speculative.
Economic analyses comparing proton therapy to conventional radiation therapy from a societal perspective must consider not only direct treatment costs but also potential savings from reduced late toxicity management. If proton therapy significantly reduces erectile dysfunction, urinary incontinence, or secondary malignancies, these benefits may offset higher initial treatment costs over a patient’s lifetime. However, robust health economic data remain limited.
Patients should discuss insurance coverage, out-of-pocket costs, and financial assistance programs with their treatment team. Some proton therapy centers offer financial counseling to help patients understand their financial obligations and identify resources to support access to treatment.
Future Directions in Prostate Cancer Treatment
The future of proton therapy for prostate cancer involves several promising developments. Research from leading technology and research institutions is exploring ultra-high dose-rate proton therapy, which may allow faster treatment delivery while potentially improving outcomes. Pencil beam scanning technology enables even more precise dose conformality than current scattering foil techniques.
Ongoing clinical trials are directly comparing proton therapy to conventional radiation therapy in randomized fashion, which will provide definitive evidence regarding superiority or equivalence of these approaches. The PROMPT trial and other prospective studies should clarify the role of proton therapy in prostate cancer management and identify patient populations most likely to benefit.
Integration of advanced imaging, including functional MRI and PET scanning, with proton therapy planning may enable better tumor delineation and treatment personalization. Biomarker-driven patient selection could eventually allow clinicians to identify which patients will benefit most from proton therapy’s dosimetric advantages based on genetic or molecular characteristics.
The field is also exploring hypofractionated proton therapy, delivering higher doses per fraction over shorter treatment courses. This approach may improve convenience for patients while potentially improving outcomes, though long-term data are still emerging. Additionally, combining proton therapy with immunotherapy or other systemic treatments represents an active area of investigation.
For healthcare professionals interested in the broader rehabilitation and supportive care landscape, exploring advanced physical therapy education provides valuable insights into helping cancer survivors manage treatment effects and optimize functional recovery.
FAQ
Is proton therapy better than traditional radiation for prostate cancer?
Proton therapy offers theoretical advantages through improved dose conformality and reduced exit dose, potentially reducing late toxicity. However, biochemical control rates are comparable to conventional radiation therapy. The choice depends on individual patient factors, disease characteristics, and institutional expertise. Prospective randomized trials are ongoing to definitively establish superiority.
What is the success rate of proton therapy for prostate cancer?
Five-year biochemical recurrence-free survival rates with proton therapy exceed 90% for low-risk disease and 80-90% for intermediate-risk disease, comparable to conventional radiation therapy outcomes. Success rates depend on disease stage, risk stratification, and treatment protocol adherence.
What are the side effects of proton therapy?
Acute side effects include urinary frequency, dysuria, and mild rectal symptoms, typically resolving within weeks. Late side effects may include erectile dysfunction, urinary incontinence, and gastrointestinal toxicity, though proton therapy generally produces lower rates of severe late toxicity compared to conventional radiation.
How long does proton therapy treatment take?
Typical proton therapy courses last 8-9 weeks with daily treatments. Some centers offer hypofractionated schedules with fewer, higher-dose treatments over 4-6 weeks. Treatment duration depends on the specific protocol and clinical circumstances.
Is proton therapy covered by insurance?
Medicare generally covers proton therapy for prostate cancer. Private insurance coverage varies and may require prior authorization. Patients should contact their insurance providers and treatment centers’ financial counseling services to understand coverage and out-of-pocket costs.
Who is the best candidate for proton therapy?
Ideal candidates include younger patients with low to intermediate-risk disease who have long life expectancies and would benefit most from reduced late toxicity risk. Patients with prior pelvic radiation or significant baseline urinary dysfunction may be poor candidates, requiring individual evaluation.
How does proton therapy compare to surgery for prostate cancer?
Both proton therapy and surgical approaches (radical prostatectomy) achieve excellent cancer control for localized disease. Proton therapy avoids surgical risks and recovery time but carries radiation-related side effects. The choice depends on patient preference, age, comorbidities, and surgeon/radiation oncologist expertise. Research institutions worldwide continue investigating optimal treatment selection strategies.



