
Is Piggyback IV Therapy Effective? Expert Insights and Evidence-Based Analysis
Piggyback IV therapy has emerged as a significant advancement in modern medical practice, offering healthcare providers and patients a more flexible and efficient approach to intravenous medication administration. This specialized technique allows secondary medications to be infused through an existing primary IV line, rather than requiring separate punctures or additional access points. Understanding the effectiveness, safety considerations, and practical applications of this method is essential for patients and medical professionals alike.
The growing adoption of piggyback IV therapy across hospitals, clinics, and home healthcare settings reflects its proven benefits in improving patient outcomes and reducing complications. As with any medical intervention, effectiveness depends on proper technique, appropriate medication selection, and careful monitoring. This comprehensive guide examines the scientific evidence, clinical applications, and expert perspectives on piggyback IV therapy to help you make informed healthcare decisions.
What Is Piggyback IV Therapy and How Does It Work
Piggyback IV therapy, also known as secondary IV infusion, represents a practical approach to administering multiple intravenous medications without requiring multiple venipunctures. The technique involves connecting a secondary IV bag or bottle to the primary IV line at an injection port, typically positioned above the primary infusion site. This configuration allows medications to flow through the same cannula while maintaining the integrity and accessibility of the primary IV line.
The mechanics of piggyback therapy rely on a carefully designed system of gravity, flow rates, and one-way valves. When the secondary medication is elevated above the primary IV bag, gravity naturally facilitates the flow of the secondary infusion. Once the secondary infusion completes, the system automatically reverts to the primary IV line, which continues delivering its designated therapy. This seamless transition eliminates the need for manual switching and reduces the risk of contamination or medication errors.
The primary IV line typically delivers maintenance fluids or a continuous medication, while the secondary line introduces additional medications that require periodic or intermittent dosing. Common scenarios include administering antibiotics every six hours while maintaining a continuous saline drip, or delivering pain medications at scheduled intervals through an existing IV access point. This flexibility makes piggyback therapy particularly valuable in hospital settings where patients require multiple medications with different schedules.

Clinical Effectiveness and Research Evidence
Extensive clinical research demonstrates that piggyback IV therapy is highly effective when properly executed. Studies published in nursing and medical journals consistently show that this method successfully delivers medications at therapeutic levels while maintaining patient safety and comfort. PubMed Central contains numerous peer-reviewed studies documenting the efficacy of secondary IV infusion techniques across various patient populations and clinical settings.
Research indicates that piggyback therapy achieves comparable medication serum levels to direct IV push administration when administered according to established protocols. A critical factor in effectiveness is adherence to proper timing and flow rate calculations. When healthcare providers follow evidence-based guidelines for medication compatibility, infusion rates, and monitoring intervals, patient outcomes remain consistently positive. Studies specifically examining antibiotic delivery through piggyback systems show bacterial eradication rates equivalent to those achieved through traditional IV push methods.
The effectiveness of piggyback therapy extends beyond simple medication delivery. Clinical data shows that this approach reduces patient anxiety associated with repeated needle sticks, improves medication adherence in outpatient settings, and decreases healthcare costs by minimizing complications related to multiple IV sites. Hospitals implementing standardized piggyback protocols report improved infection control metrics and reduced catheter-related bloodstream infections.
Expert consensus from major nursing organizations supports piggyback IV therapy as an evidence-based practice when appropriate medications are selected and proper technique is maintained. The Oncology Nursing Society and similar professional organizations include piggyback administration in their clinical practice guidelines for safe medication administration.
Advantages Over Traditional IV Administration
Piggyback IV therapy offers numerous clinical and practical advantages that have contributed to its widespread adoption in modern healthcare settings. The most obvious benefit is the reduction in needle sticks and venipunctures required for patients receiving multiple medications. This advantage becomes particularly significant for patients with difficult venous access, elderly patients with fragile veins, or those requiring extended hospitalization.
Patient comfort represents another substantial advantage of this delivery method. Reducing the number of IV sites decreases pain, bruising, and the psychological stress associated with repeated needle procedures. Patients report higher satisfaction levels when receiving multiple medications through a single access point rather than enduring multiple punctures. This improved patient experience can lead to better compliance with treatment regimens and faster overall recovery.
Cost-effectiveness constitutes a major advantage for healthcare systems. Piggyback therapy reduces the supplies required for multiple IV sites, decreases nursing time spent on venipunctures, and minimizes complications that would require additional treatment and hospitalization. When considering the broader healthcare economics, the savings from reduced infection rates and shorter hospital stays far exceed the minimal additional cost of secondary infusion equipment.
The flexibility of piggyback administration allows healthcare providers to adjust medication schedules without disrupting the patient’s primary IV therapy. This adaptability proves invaluable in dynamic clinical environments where treatment plans frequently change based on patient response and evolving clinical conditions. Additionally, this method maintains better infection control by limiting the number of potential entry points into the vascular system.
Piggyback therapy also facilitates better medication timing and scheduling. Nurses can administer secondary medications at precisely calculated intervals without waiting for previous medications to be fully metabolized or cleared. This precision is particularly important for time-sensitive medications where therapeutic drug levels depend on consistent dosing intervals.
Safety Considerations and Potential Risks
While piggyback IV therapy is generally safe when properly administered, healthcare providers and patients should understand potential risks and mitigation strategies. Medication incompatibility represents the most significant concern, as combining certain drugs can result in precipitation, reduced efficacy, or harmful chemical reactions. Comprehensive drug compatibility charts and institutional protocols must guide all piggyback therapy decisions.
Infection risk, while lower than with multiple IV sites, still requires vigilant monitoring. The secondary injection port introduces a potential entry point for bacteria if aseptic technique is not maintained during setup and administration. Healthcare providers must use sterile technique when connecting secondary lines and regularly inspect the insertion site for signs of infection, inflammation, or infiltration.
Phlebitis, an inflammation of the vein, can occur with piggyback therapy, particularly when irritating medications are administered or when the catheter remains in place for extended periods. Careful site assessment, appropriate catheter sizing, and adherence to dwell time guidelines help prevent this complication. Patients should be educated to report pain, swelling, redness, or warmth at the IV site immediately.
Flow rate errors can compromise medication effectiveness or cause adverse reactions if secondary infusions are delivered too rapidly. Proper calculation of infusion rates based on medication concentration, patient weight, and clinical indication is essential. Infusion pumps with programmed parameters help prevent errors, though nursing assessment and verification remain critical safeguards.
Backflow of primary medication into the secondary line can occur if the secondary infusion is not elevated appropriately or if one-way valves malfunction. This backflow may dilute secondary medications or introduce incompatible substances into the secondary infusion, potentially compromising therapy. Regular equipment inspection and proper setup protocols prevent this complication.
Air embolism, though rare, represents a serious potential complication. Proper priming of secondary lines and careful monitoring for air bubbles during setup and administration are essential safety measures. Healthcare providers must verify that all connections are secure and that no air enters the vascular system during medication administration.
Common Medications Used in Piggyback Therapy
Numerous medications are appropriately administered via piggyback therapy, with antibiotics representing the most common category. Beta-lactam antibiotics, fluoroquinolones, and aminoglycosides are routinely delivered through secondary infusions in hospital and outpatient settings. The intermittent dosing schedule typical of antibiotic therapy makes piggyback administration particularly suitable for these medications.
Chemotherapy agents represent another important category of medications administered via piggyback systems. Cancer centers and oncology units frequently utilize secondary infusions for delivering cytotoxic drugs while maintaining primary hydration lines. This approach allows precise control over medication delivery while protecting the vein with continuous saline irrigation between doses.
Antiviral medications, including antiretroviral therapies and agents for treating viral infections, are commonly given as piggyback infusions. These medications often require specific timing and intervals that are easily managed through secondary IV lines. Pain medications, antiemetics, and other supportive care drugs are also frequently administered via this method.
Electrolyte replacements and nutritional supplements may be delivered through piggyback systems when rapid correction is needed or when the medication requires careful monitoring. Immunoglobulin preparations and blood products sometimes utilize secondary infusions, though specific institutional protocols and compatibility considerations must be verified before administration.
Vasoactive medications and cardiac drugs occasionally require piggyback administration in critical care settings, though these high-risk medications typically demand more intensive monitoring and often utilize dedicated lines. Healthcare providers must verify medication compatibility and stability before combining any substances in a piggyback system.
Best Practices for Implementation
Successful piggyback IV therapy implementation requires adherence to evidence-based best practices established by nursing organizations and infection control experts. Comprehensive staff education represents the foundation of safe practice, ensuring that all healthcare providers understand proper technique, medication compatibility, and monitoring requirements. Regular competency assessments help maintain consistent quality across all clinical staff.
Standardized protocols and order sets reduce variability and medication errors in piggyback administration. Institutions should develop clear guidelines specifying which medications are appropriate for piggyback delivery, required infusion times, and mandatory monitoring intervals. Electronic health records systems can incorporate these protocols, providing real-time decision support for prescribing and administering providers.
Medication compatibility verification must occur before every piggyback infusion. Pharmacists play a crucial role in reviewing orders and confirming that primary and secondary medications can be safely co-administered. Institutional drug compatibility databases and published references provide evidence-based information for these critical decisions.
Proper setup technique is essential for safe piggyback therapy. Secondary bags should be positioned 6-12 inches above the primary IV bag to ensure gravity-driven flow. All connections must be secure and sterile, with appropriate use of sterile gauze or alcohol wipes at injection ports. The secondary tubing should be primed before connection to the primary line to prevent air introduction.
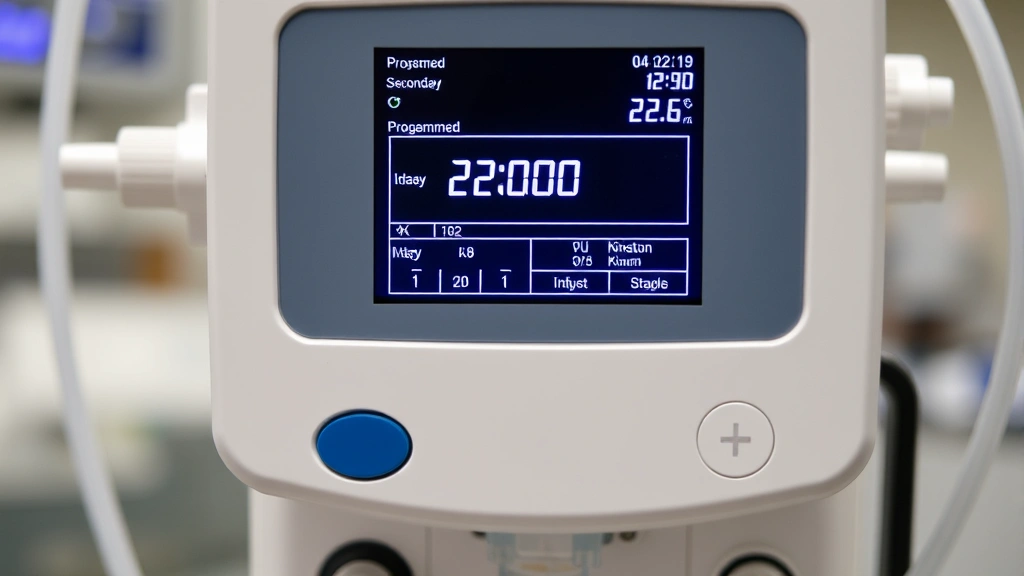
Infusion pump programming ensures accurate medication delivery at prescribed rates. Most modern pumps allow secondary infusion programming with automatic return to primary infusion after the secondary dose completes. Nurses should verify pump settings before initiating therapy and monitor the infusion at regular intervals.
Documentation of piggyback infusions should include medication name and dose, infusion time, rate, and patient response. Nursing notes should reflect assessment findings, any complications or adverse reactions, and patient tolerance of the therapy. This comprehensive documentation supports continuity of care and provides important data for evaluating therapy effectiveness.
Comparison with Other Delivery Methods
Piggyback IV therapy occupies an important position within the spectrum of intravenous medication delivery options, each with distinct advantages and limitations. Direct IV push administration, where medications are injected directly into the vein through a syringe, offers rapid onset but requires careful technique to prevent vascular injury and provides less control over infusion rate. This method is suitable for medications requiring quick action but unsuitable for irritating substances or large volumes.
Continuous IV infusion, where medications are delivered over extended periods through gravity or pump-controlled systems, provides steady drug levels and is ideal for maintenance therapy. However, continuous infusion limits flexibility when medication changes are needed and may deliver unnecessarily high total doses if only intermittent therapy is required. Patients receiving prolonged IV therapy often benefit from the flexibility that piggyback systems provide.
Peripheral IV lines, the most common vascular access method, have limited capacity for delivering multiple medications simultaneously. Piggyback therapy maximizes the utility of peripheral access by allowing multiple medications without additional punctures. Central venous catheters offer superior access for patients requiring extensive IV therapy but carry higher infection and complication risks, making them unsuitable for patients needing only periodic medication administration.
Intramuscular and subcutaneous injection represent alternative routes for many medications, avoiding vascular access altogether. However, these routes may be unsuitable for large volumes, irritating medications, or patients with coagulation disorders. Oral medication administration, when feasible, offers convenience and reduced infection risk but provides less precise control over drug absorption and timing.
Home-based IV therapy programs frequently utilize piggyback systems because of their simplicity, safety profile, and compatibility with portable infusion pumps. Patients managing chronic conditions requiring periodic IV medications benefit from the flexibility and reduced healthcare facility visits that this delivery method enables. Telehealth monitoring programs increasingly support home-based IV therapy, making piggyback administration accessible to patients in diverse settings.
The choice among delivery methods depends on medication properties, patient factors, clinical setting, and treatment goals. Piggyback therapy often represents the optimal balance between safety, efficacy, and practical feasibility for patients requiring multiple intermittent medications. Healthcare providers should evaluate individual patient circumstances when selecting the most appropriate delivery method.
Frequently Asked Questions
How long does a piggyback IV infusion typically take?
Piggyback infusion duration varies depending on medication type, concentration, and prescribed infusion rate. Most piggyback medications infuse over 15-60 minutes, though some may require longer periods. The prescribing physician specifies the infusion time based on medication pharmacokinetics and clinical indication. Nurses calculate infusion rates to deliver the prescribed dose within the specified timeframe.
Can all medications be given as piggyback infusions?
Not all medications are suitable for piggyback administration. Medications must be compatible with the primary IV solution and other co-administered drugs. Some medications require dedicated lines due to incompatibility or the need for precise monitoring. Healthcare providers consult drug compatibility charts and pharmacist recommendations before deciding whether piggyback administration is appropriate for specific medications.
What should patients do if they experience pain or swelling at the IV site during piggyback infusion?
Patients should immediately notify their healthcare provider if they experience pain, swelling, redness, warmth, or other concerning symptoms at the IV site. These symptoms may indicate infiltration, phlebitis, or infection requiring prompt intervention. Healthcare providers assess the site and may need to relocate the IV catheter to a new site if complications are identified.
Is piggyback IV therapy more expensive than other delivery methods?
While piggyback therapy requires slightly more equipment than simple continuous infusions, it typically costs less overall than alternative delivery methods requiring multiple IV sites or more intensive monitoring. The reduced need for venipunctures, lower complication rates, and decreased nursing time for site care make piggyback therapy cost-effective for most applications. Insurance coverage for piggyback administration is standard in most healthcare settings.
How do healthcare providers prevent medication incompatibility problems in piggyback therapy?
Pharmacists review all medication orders to verify compatibility before administration. Institutions maintain comprehensive drug compatibility databases and reference materials. When compatibility is uncertain, medications may be flushed between infusions or delivered through separate lines. Nursing staff receive training on recognizing signs of incompatibility, such as precipitation, discoloration, or unusual odors.
Can patients receiving supportive therapies also use piggyback IV administration?
Yes, patients receiving various supportive treatments, including physical and occupational therapies, can safely receive piggyback IV medications. The combination of therapies requires coordination among healthcare team members to ensure optimal timing and minimize disruptions to treatment schedules. Piggyback therapy’s flexibility actually facilitates integration with other therapeutic interventions.
What training do nurses require to safely administer piggyback IV therapy?
Nurses must complete comprehensive training covering medication compatibility, aseptic technique, infusion rate calculations, and monitoring protocols. Initial competency assessment through supervised practice ensures nurses can safely perform all aspects of piggyback administration. Ongoing education keeps staff updated on new medications, equipment, and best practice guidelines. Annual competency reassessment maintains consistent quality standards.
How does piggyback therapy compare to other therapeutic modalities in terms of patient satisfaction?
Patient satisfaction with piggyback therapy is generally high because it reduces needle sticks, minimizes pain and bruising, and requires less time spent in healthcare settings. Patients appreciate the convenience of single-site IV access and the flexibility it provides for their daily activities. Satisfaction scores are particularly high among patients requiring extended treatment periods or frequent medication administration.
What signs indicate that a piggyback infusion is not working properly?
Healthcare providers monitor for several indicators of improper infusion, including failure of the secondary medication to infuse at the expected rate, backflow of primary solution into secondary tubing, or the secondary infusion completing significantly faster or slower than calculated. Alarm sounds from infusion pumps may indicate air in the line, occlusion, or other problems. Nurses should immediately investigate and correct any abnormalities.



