Laser Therapy for Gums: Dentist Insights on Periodontal Treatment
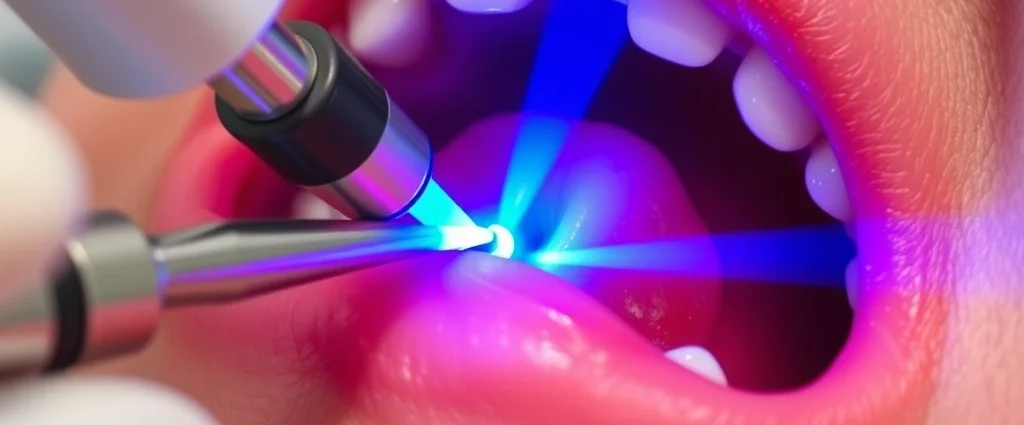
Laser therapy has revolutionized modern dentistry, offering patients a minimally invasive alternative to traditional gum disease treatment. Periodontal disease affects millions of people worldwide, ranging from mild gingivitis to severe periodontitis that can lead to tooth loss and bone deterioration. Dentists increasingly turn to laser technology to treat these conditions with precision, reduced pain, and faster healing times compared to conventional surgical methods.
The application of lasers in periodontal therapy represents a significant advancement in dental science. Unlike traditional scaling and root planing, which rely on mechanical instruments to remove tartar and bacteria from below the gum line, laser for periodontal therapy uses concentrated light energy to eliminate diseased tissue and pathogens. This targeted approach minimizes damage to healthy tissue, reduces bleeding, and promotes natural healing processes. Understanding how laser therapy works and its benefits can help patients make informed decisions about their gum health.

How Laser Therapy Works for Periodontal Disease
Laser technology in periodontal therapy operates on principles of photothermal and photochemical interactions with oral tissues. When a dentist directs laser energy into the periodontal pocket—the space between the tooth and gum where bacteria accumulate—the light energy is absorbed by pigmented bacterial cells and hemoglobin in blood vessels. This absorption generates heat that destroys pathogenic bacteria, inflammatory tissue, and calculus deposits without requiring aggressive mechanical removal.
The wavelength of the laser determines its penetration depth and interaction with different tissue types. Most dental lasers operate in the infrared spectrum, allowing them to penetrate several millimeters below the gum surface while remaining safe for surrounding tissues. The laser’s energy also stimulates fibroblast activity, which promotes collagen production and tissue regeneration. This biological response accelerates healing and can lead to reattachment of gum tissue to the tooth root—a critical outcome in periodontal therapy.
Beyond bacterial elimination, laser therapy reduces inflammation by decreasing pro-inflammatory cytokines and promoting anti-inflammatory responses. This immunomodulatory effect provides benefits that extend beyond the immediate treatment period. Patients often experience reduced bleeding, decreased pocket depths, and improved overall periodontal health within weeks of laser treatment.

Types of Lasers Used in Dental Practice
Several laser systems have demonstrated efficacy in periodontal applications, each with distinct characteristics. The Nd:YAG (neodymium-doped yttrium aluminum garnet) laser operates at 1064 nanometers wavelength and effectively targets pigmented bacterial cells and hemoglobin. Many periodontists prefer Nd:YAG lasers for their superior bactericidal effects and tissue penetration capabilities. The FDA has cleared multiple Nd:YAG systems specifically for periodontal therapy.
Diode lasers, operating between 810-980 nanometers, offer excellent portability and are increasingly popular in general dental practices. These lasers provide good bacterial elimination with shorter treatment times and lower cost compared to larger systems. The 980-nanometer diode laser shows particular promise for pocket sterilization and biofilm removal.
Erbium lasers (Er:YAG and Er,Cr:YSGG) operate at longer wavelengths and are highly absorbed by water in tissues. While primarily used for hard tissue ablation, some erbium systems have been adapted for soft tissue periodontal applications. CO2 lasers, though effective for some dental procedures, are less commonly used in periodontal therapy due to their limited penetration depth.
The choice between laser types depends on clinical goals, tissue characteristics, and the specific periodontal condition being treated. Many modern dental facilities invest in comprehensive therapy resources to train practitioners in multiple laser modalities.
Clinical Benefits and Treatment Outcomes
Peer-reviewed research demonstrates significant clinical advantages when using laser therapy for periodontal conditions. Studies published in journals like the Journal of Periodontology and Lasers in Surgery and Medicine show that laser-assisted periodontal therapy achieves superior clinical attachment level gains compared to conventional scaling and root planing alone.
Patients undergoing laser treatment typically experience greater pocket depth reduction—often 2-3 millimeters more than conventional therapy. This outcome translates to improved periodontal health and reduced risk of disease progression. Clinical attachment gains, which measure actual reattachment of gum tissue to tooth roots, are consistently higher with laser-assisted approaches, indicating true regeneration rather than superficial healing.
Bleeding on probing, a key indicator of gum inflammation, decreases dramatically following laser therapy. Many patients report elimination of bleeding within 2-4 weeks post-treatment. This improvement reflects both the antimicrobial effects and the anti-inflammatory response triggered by laser energy.
Long-term follow-up studies spanning 6-12 months show sustained benefits, with many patients maintaining improved periodontal parameters without additional intervention. For patients with moderate to advanced periodontitis, laser therapy often provides outcomes comparable to traditional surgical flap procedures but with significantly less post-operative discomfort and faster healing.
Comparison with Traditional Gum Treatment Methods
Traditional periodontal treatment relies primarily on mechanical instrumentation—scaling and root planing—performed manually or with ultrasonic instruments. While effective, these mechanical approaches require aggressive manipulation of tissues to remove calculus and diseased material. This mechanical trauma inevitably causes tissue disruption, increased bleeding, and longer recovery periods.
Conventional surgical approaches, such as flap surgery for advanced cases, involve incising gum tissue, reflecting it to access deeper roots, and removing diseased tissue manually. These procedures are highly effective but carry substantial morbidity—patients experience significant pain, swelling, and extended recovery times. Many patients avoid necessary periodontal treatment due to fear of surgical intervention.
Laser therapy eliminates the need for aggressive mechanical removal by using energy-based ablation. The precision of laser delivery means healthy tissue remains largely undisturbed while pathogenic material is selectively eliminated. This selective targeting reduces trauma and associated complications. Additionally, laser therapy can be performed without local anesthesia in many cases, though most practitioners still use numbing agents for patient comfort.
The non-surgical nature of laser therapy makes it particularly attractive for patients with medical conditions that complicate healing, such as diabetes or immunosuppression. While laser therapy isn’t universally superior for every patient or condition, it represents an excellent option for many cases and often serves as a valuable adjunct to conventional approaches. For additional context on minimally invasive therapeutic approaches, consider exploring resources on physical therapy techniques that similarly emphasize non-invasive treatment.
Key advantages of laser therapy include:
- Minimal tissue trauma and faster healing
- Reduced post-operative pain and swelling
- Improved patient comfort during treatment
- Enhanced antimicrobial effects
- Stimulation of tissue regeneration
- Reduced bleeding and inflammation
- Lower infection risk due to sterilization
- Ability to treat multiple sites in single appointment
Patient Experience and Recovery
The patient experience during laser periodontal therapy differs markedly from traditional surgical approaches. Most patients report minimal discomfort during the procedure, often describing only mild warmth or slight vibration sensations. The absence of mechanical pressure and tissue manipulation makes the experience psychologically less stressful than traditional surgery.
Post-operative recovery is substantially faster with laser therapy. While traditional flap surgery may require 2-3 weeks for initial healing and several months for complete resolution, laser-treated patients typically return to normal activities within 24-48 hours. Swelling and discomfort are minimal in most cases, allowing patients to maintain regular oral hygiene routines immediately post-treatment.
Pain management after laser therapy is typically minimal. Most patients require only over-the-counter analgesics if any medication at all. This contrasts sharply with conventional surgery, where prescription-strength pain medication is often necessary for several days. The reduced pain and rapid recovery significantly improve patient compliance with post-treatment care instructions.
Dietary restrictions are minimal following laser therapy. Patients can usually resume normal eating habits immediately, whereas surgical patients often face 1-2 weeks of soft diet recommendations. This rapid return to normalcy improves quality of life and patient satisfaction with treatment.
The psychological impact of treatment cannot be overlooked. Fear of dental surgery prevents many patients from seeking necessary periodontal care. Laser therapy’s non-surgical nature and rapid recovery appeal to anxious patients, potentially increasing treatment acceptance rates. Many dental offices now emphasize the psychological benefits of anxiety reduction associated with less invasive procedures.
Cost Considerations and Insurance Coverage
Laser periodontal therapy typically costs more than conventional scaling and root planing but often less than traditional surgical approaches. Average costs range from $800-$2,000 per session depending on the extent of treatment and geographic location. While this represents a significant investment, many patients find the value proposition compelling when considering reduced recovery time and improved outcomes.
Insurance coverage varies considerably. Some dental insurance plans classify laser therapy as a standard periodontal procedure and provide coverage similar to conventional treatment. Others categorize it as an elective or experimental treatment, resulting in lower reimbursement rates or no coverage. Patients should verify their specific coverage before committing to treatment.
Many dental practices offer payment plans or financing options to make laser therapy accessible. Some also bundle laser treatment with conventional scaling and root planing, creating comprehensive packages at reasonable cost. Direct-pay dental plans and dental discount programs increasingly cover laser periodontal therapy as practitioners recognize its efficacy and popularity.
The long-term cost-benefit analysis often favors laser therapy. Superior clinical outcomes reduce the need for repeated treatments or advanced surgical intervention. Patients who maintain excellent oral hygiene following laser therapy frequently avoid progression to more expensive treatments. Additionally, preventing tooth loss through effective periodontal treatment saves substantial costs associated with tooth replacement options like implants or bridges.
Safety and Potential Risks
Laser therapy for periodontal disease has an excellent safety profile when administered by trained professionals. The FDA has cleared multiple laser systems for periodontal use based on rigorous clinical evidence. However, like any medical procedure, certain risks and considerations exist.
Thermal injury is the primary concern with laser therapy. Improper technique, excessive energy delivery, or inadequate cooling can damage healthy tissue. Trained practitioners use appropriate energy settings, cooling mechanisms, and treatment protocols to minimize this risk. Most modern dental lasers include safety features like automatic shutoff and real-time power monitoring.
Eye safety requires attention during laser procedures. Both patients and clinicians must wear appropriate laser safety glasses to prevent retinal damage. Dental practices using laser equipment maintain strict safety protocols and train all staff members in proper safety procedures.
Infection risk is minimal with laser therapy compared to conventional surgery due to the sterilizing effect of laser energy. The antimicrobial action actually reduces infection likelihood. However, patients must still follow post-operative care instructions to prevent secondary infection.
Contraindications are relatively few. Patients with certain medications, such as photosensitizing agents, require special consideration. Pregnant women are typically advised to postpone elective laser treatment, though some practitioners treat pregnant patients for urgent periodontal conditions. Patients with active oral infections may benefit from antibiotic pretreatment before laser therapy.
Research from peer-reviewed dental journals consistently demonstrates safety when laser therapy follows established protocols. Complications are rare when practitioners receive proper training and maintain appropriate equipment maintenance schedules.
Evidence-Based Outcomes and Research
Scientific evidence supporting laser therapy for periodontal disease continues to accumulate. Meta-analyses published in leading dental journals demonstrate that laser-assisted treatment produces superior clinical outcomes compared to conventional scaling and root planing alone. Studies examining lasers in surgery and medicine show consistent benefits across multiple laser types and patient populations.
Randomized controlled trials, considered the gold standard in clinical research, show that laser therapy achieves greater probing depth reduction and clinical attachment level gains. These objective measures of periodontal health improvement indicate that laser treatment produces real regeneration of supporting tissues, not merely cosmetic improvement.
Research also documents the biological mechanisms underlying laser therapy’s success. Studies using molecular and cellular techniques reveal that laser energy stimulates specific growth factors, reduces inflammatory markers, and enhances angiogenesis—the formation of new blood vessels supporting tissue healing. Understanding these mechanisms validates laser therapy as a legitimate biological treatment rather than merely a novelty.
Comparative effectiveness research demonstrates that laser therapy achieves outcomes comparable to traditional surgical flap procedures in many cases, with substantially reduced patient morbidity. This finding has important implications for clinical decision-making, as it suggests laser therapy should be considered as a primary treatment option rather than a last resort.
Long-term studies examining patient outcomes 1-2 years post-treatment show sustained benefits, indicating that laser therapy produces durable improvements in periodontal health. These findings support laser therapy as a legitimate long-term solution rather than a temporary fix requiring repeated interventions.
Frequently Asked Questions
Is laser therapy painful?
Most patients experience minimal discomfort during laser periodontal therapy. The procedure typically causes only mild sensations of warmth or slight vibration. Local anesthesia is usually applied for patient comfort, though many patients note they would not require numbing agents. Post-operative pain is generally minimal, rarely requiring more than over-the-counter pain medication.
How long does treatment take?
Laser periodontal therapy typically requires 1-2 hours depending on the extent of disease and number of teeth affected. The procedure can often be completed in a single appointment or two appointments spaced 1-2 weeks apart. This is considerably faster than traditional flap surgery, which may require multiple appointments and longer healing time.
What is the success rate of laser therapy?
Clinical studies demonstrate success rates of 70-90% for achieving significant periodontal improvement with laser therapy. Success is measured by reduced pocket depths, clinical attachment level gains, and resolution of bleeding. Patient compliance with post-treatment oral hygiene and maintenance care significantly influences long-term success.
Can laser therapy replace traditional gum surgery?
Laser therapy can replace traditional surgery in many cases, particularly for moderate periodontitis. However, advanced cases with severe bone loss may still require surgical approaches. Many periodontists use laser therapy as the first-line treatment, reserving surgery for cases showing inadequate response. The choice depends on disease severity, patient factors, and clinical judgment.
Will my insurance cover laser therapy?
Insurance coverage varies significantly. Some plans cover laser therapy as a standard periodontal procedure, while others provide limited or no coverage. Contact your insurance provider with your dentist’s procedure code to determine your specific coverage. Many dental practices offer financing options to make treatment accessible regardless of insurance coverage.
How long does improvement take after laser treatment?
Patients typically notice initial improvements within 1-2 weeks, with continued improvement over 2-3 months. Bleeding on probing often resolves within 2-4 weeks. Maximum clinical benefits, including complete tissue remodeling and attachment gain, may require 3-6 months. Regular follow-up appointments monitor progress and ensure optimal outcomes.
Are there any side effects?
Side effects are minimal with laser therapy. Temporary mild sensitivity or slight gum tenderness may occur but typically resolves within 24-48 hours. Serious complications are rare when the procedure follows established safety protocols. Most patients tolerate laser therapy better than conventional surgical approaches.
Do I still need to floss after laser treatment?
Yes, excellent oral hygiene is critical following laser therapy. Flossing, brushing, and regular professional cleanings help maintain the improvements achieved through laser treatment. Many periodontists emphasize that laser therapy is most effective when combined with superior home care and professional maintenance.
For additional information on therapeutic approaches and treatment options, explore our resources on occupational therapy careers and music therapy services that emphasize comprehensive wellness approaches similar to modern periodontal care.
Selecting a Qualified Laser Therapy Provider
Choosing a dentist or periodontist experienced in laser therapy is crucial for optimal outcomes. Look for practitioners who have completed formal training in laser periodontal techniques through accredited dental organizations. Board certification in periodontics, combined with specific laser training, indicates advanced expertise.
Ask potential providers about their experience with laser therapy, including the number of cases treated and patient outcomes. Inquire about the specific laser system used and why they selected that technology. Reputable practitioners welcome questions and provide detailed information about their approach.
Review before-and-after photos and patient testimonials to assess the quality of outcomes. Many experienced providers maintain portfolios demonstrating clinical results. Reading patient reviews on dental websites and practice websites provides insight into patient satisfaction and experience.
Ensure the practice maintains proper safety protocols, including laser safety certifications for staff members and appropriate safety equipment. A well-organized practice demonstrates commitment to patient safety and clinical excellence. Don’t hesitate to ask about maintenance schedules for laser equipment and quality assurance measures.
Consultation appointments allow you to discuss your specific periodontal condition and determine whether laser therapy is appropriate for your situation. A thorough evaluation, including periodontal probing and possibly imaging, helps establish baseline measurements to assess treatment effectiveness.
The Future of Laser Periodontal Therapy
Technological advances continue to expand laser therapy capabilities and improve clinical outcomes. Emerging research explores combination approaches pairing laser therapy with regenerative materials, photodynamic therapy, and antimicrobial peptides to enhance periodontal regeneration. These innovative approaches show promise for even superior outcomes in future years.
Artificial intelligence and digital imaging technologies are beginning to integrate with laser therapy, allowing for more precise treatment planning and real-time monitoring of tissue response. These developments may further improve clinical outcomes and treatment efficiency.
As evidence accumulates and more practitioners gain training, laser therapy is becoming increasingly mainstream in periodontal care. Insurance coverage is gradually expanding as payers recognize the clinical efficacy and long-term cost benefits. The trend toward laser-based approaches reflects the dental profession’s evolution toward minimally invasive, biologically-sound treatment modalities.
Patient awareness and demand for laser therapy continues growing as word spreads about superior outcomes and minimal recovery time. This patient demand drives adoption among dental practitioners and encourages continued research into laser applications. The future of periodontal care increasingly centers on precision, biology-based approaches exemplified by laser therapy.
For comprehensive information on modern laser periodontal techniques, consult resources from professional dental organizations and published research in peer-reviewed journals. Additionally, red light therapy research demonstrates broader applications of light-based healing modalities across medical disciplines, validating the biological principles underlying laser therapy effectiveness.