Trigger Finger Relief: What Experts Recommend
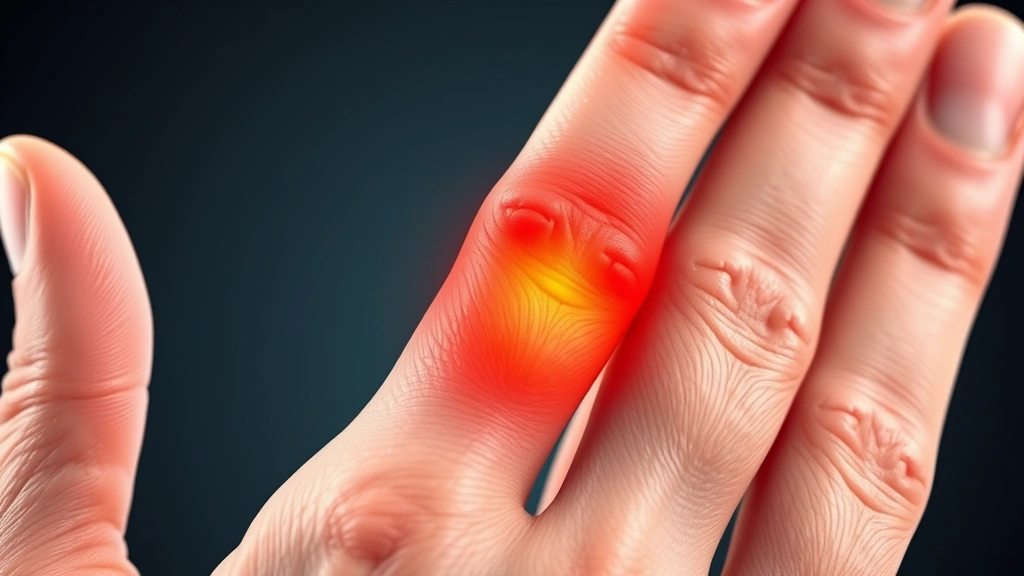
Trigger finger, medically known as stenosing tenosynovitis, is a painful condition affecting the hand where one or more fingers become stuck in a bent position before suddenly straightening with a snap—similar to a trigger being pulled. This common hand disorder occurs when inflammation narrows the sheath surrounding the tendon, restricting smooth movement. The condition affects millions of people worldwide, with higher prevalence in individuals aged 40-60 and those with diabetes or rheumatoid arthritis.
Understanding trigger finger therapies and expert-recommended treatments can help you manage pain, restore function, and prevent long-term complications. Whether you’re experiencing mild symptoms or severe restrictions, this comprehensive guide explores evidence-based approaches that healthcare professionals recommend for relief and recovery.

Understanding Trigger Finger: Causes and Symptoms
Trigger finger develops when the pulley system that guides tendons through the hand becomes inflamed or thickened. The flexor tendons, which control finger bending, run through a series of pulleys in the palm and fingers. When the sheath surrounding these tendons swells, the tendon cannot glide smoothly through the narrowed space, creating the characteristic catching and snapping sensation.
Several risk factors increase the likelihood of developing this condition. Repetitive gripping activities, forceful use of the fingers, and prolonged pressure on the palm can all contribute to inflammation. Individuals with diabetes experience trigger finger at significantly higher rates due to altered collagen in tendons. Rheumatoid arthritis and other inflammatory conditions predispose people to this disorder, as does female gender and advancing age.
Common symptoms include morning stiffness in the affected finger, pain in the palm at the base of the finger, swelling or tenderness, and the characteristic locking sensation. In mild cases, symptoms appear primarily in the morning and improve throughout the day. Severe cases involve persistent locking that may require manual straightening of the finger, causing significant pain and functional limitation.
Early recognition of symptoms enables prompt intervention with therapy resources and information that can prevent progression. Consulting healthcare providers at the first sign of persistent finger catching ensures access to appropriate treatment strategies tailored to your specific situation.

Conservative Treatment Approaches
Most experts recommend starting with conservative, non-invasive treatments that address inflammation and allow the tendon sheath to heal naturally. These first-line interventions prove effective in approximately 60-70% of cases, particularly when implemented early in the condition’s course.
Rest and Activity Modification
Reducing activities that exacerbate symptoms represents the foundation of conservative care. This involves identifying specific movements or gripping patterns that trigger pain and consciously modifying how you perform daily tasks. Avoiding forceful gripping, prolonged pinching, and repetitive finger flexion gives the inflamed tendon sheath opportunity to heal. Many people find that simply being more mindful of hand usage provides significant relief within weeks.
Anti-Inflammatory Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen reduce inflammation and pain associated with trigger finger. These medications work by inhibiting prostaglandins and reducing swelling in the tendon sheath. Taking NSAIDs as directed for 2-4 weeks often produces noticeable improvement. However, long-term NSAID use requires medical supervision due to potential gastrointestinal and cardiovascular effects.
Splinting and Immobilization
Night splints that keep the affected finger in a slightly extended position during sleep prevent the tendon from becoming locked in the flexed position overnight. By reducing nighttime stress on the inflamed sheath, splints decrease morning stiffness and pain. Many patients wear splints for 4-6 weeks and experience substantial symptom improvement. Custom-fitted splints from occupational therapists provide optimal support compared to generic options.
Ice and Heat Therapy
Applying ice for 15-20 minutes several times daily reduces acute inflammation and pain. This works particularly well immediately after activities that aggravate symptoms. Some patients find alternating between ice and heat therapy beneficial—ice for inflammation, heat for muscle relaxation and improved circulation. Consistent application over several weeks supports the healing process.
Physical Therapy and Hand Exercises
Structured physical therapy treatment specifically designed for hand conditions helps restore function and prevent recurrence. Licensed physical therapists and occupational therapists develop personalized exercise programs that address the underlying biomechanical issues contributing to trigger finger.
Tendon Gliding Exercises
These specialized movements promote smooth tendon movement through the sheath without forcing the finger through a locked position. Tendon gliding exercises involve moving fingers through a series of positions—from straight, to hooked fist, to full fist—in controlled, pain-free ranges of motion. Performing these exercises 3-4 times daily for 5-10 repetitions each helps maintain tendon mobility and prevents adhesions from forming.
Stretching and Flexibility Work
Gentle stretching of the flexor tendons and muscles in the forearm reduces tension that contributes to trigger finger. A therapist teaches proper stretching techniques to avoid overstressing the healing tendon. Stretches held for 15-30 seconds, repeated 2-3 times, improve overall hand and forearm flexibility. Regular stretching prevents the condition from returning after initial treatment.
Strengthening Exercises
Once acute inflammation subsides, progressive strengthening exercises rebuild hand and forearm strength without re-triggering symptoms. Resistance exercises using therapy putty, grip strengtheners, or light weights should be introduced gradually under professional guidance. Building functional strength reduces compensatory movement patterns that perpetuate inflammation.
Ergonomic Education
Therapists assess how you perform daily activities and recommend modifications to reduce hand stress. This includes proper keyboard and mouse positioning, correct gripping techniques, and strategies for protecting your hands during work and recreation. Understanding ergonomic principles prevents recurrence after treatment resolves initial symptoms.
Medical Interventions and Injections
When conservative treatments provide insufficient relief after 4-6 weeks, medical professionals often recommend corticosteroid injections directly into the tendon sheath. These injections deliver powerful anti-inflammatory medication precisely where inflammation occurs, often providing dramatic symptom relief.
Corticosteroid Injections
Steroid injections reduce inflammation in the tendon sheath and surrounding tissues, allowing the tendon to glide more freely. Success rates range from 50-90% depending on disease severity and duration. Research published in medical journals demonstrates that early injection, combined with activity modification, produces the best outcomes. Most patients experience symptom improvement within 1-2 weeks of injection.
Multiple injections may be necessary—typically 2-3 injections spaced 4-6 weeks apart—to achieve lasting relief. The procedure involves minimal discomfort and can be performed in an office setting. Temporary increased symptoms lasting 24-48 hours sometimes occur as inflammation temporarily increases before subsiding.
Platelet-Rich Plasma (PRP) and Biologics
Emerging regenerative medicine approaches use PRP and other biologic agents to promote tendon healing. These newer treatments harness the body’s natural healing mechanisms by concentrating growth factors and healing compounds. While promising, these options require further research and may not be covered by insurance. Specialists in sports medicine and orthopedics increasingly offer these treatments.
Hyaluronic Acid Injections
Some practitioners recommend hyaluronic acid injections to improve tendon sheath lubrication. This substance naturally occurs in joint fluid and reduces friction during movement. While research shows potential benefits, hyaluronic acid injections are less established than corticosteroid injections for trigger finger treatment.
Surgical Options for Severe Cases
Surgical intervention becomes necessary when conservative and medical treatments fail to provide relief, or when symptoms severely limit hand function. Surgical release of the trigger finger has high success rates and provides permanent relief for most patients.
Percutaneous Release
This minimally invasive procedure uses a needle to break apart scar tissue and adhesions without making a large incision. Performed under local anesthesia, percutaneous release offers quick recovery and minimal scarring. However, recurrence rates are slightly higher than with open surgery, and it may not be suitable for all cases.
Open Surgical Release
The gold standard surgical approach involves making a small incision in the palm to access the constricted pulley and carefully divide it. This allows the tendon to move freely through the sheath. The procedure takes only 10-15 minutes and is performed under local or regional anesthesia. Recovery typically takes 2-4 weeks, with most patients achieving complete symptom resolution.
Success rates exceed 95% with open release, and recurrence is uncommon (less than 5%). Potential complications include infection, nerve damage, and reduced grip strength, though these occur in less than 2% of cases. Proper post-operative care and hand therapy optimize outcomes.
Endoscopic Release
Some surgeons use endoscopic techniques, viewing the surgical site through a small camera while performing the release through minimal incisions. This approach combines benefits of open and percutaneous procedures, offering excellent visualization with minimal tissue trauma and quick recovery.
Preventive Strategies and Lifestyle Modifications
Preventing trigger finger recurrence or initial occurrence involves modifying activities and protecting hand health. People with risk factors should implement preventive strategies before symptoms develop.
Activity Modification and Ergonomics
Proper ergonomic setup at work prevents repetitive strain injuries affecting the hand. Keyboard and mouse positioning should maintain neutral wrist alignment. Regular breaks from repetitive gripping activities allow tissue recovery. Varying tasks throughout the day prevents overuse of specific hand structures. When engaging in hobbies or sports involving repetitive hand use, proper technique and appropriate equipment reduce injury risk.
Hand Protection During Work
Workers in trades involving prolonged gripping should wear padded gloves that reduce pressure on the palm. Taking frequent breaks during activities requiring sustained gripping prevents inflammation development. Alternating between different hand positions and grip types distributes stress across different structures.
Inflammation Management
Maintaining overall health supports tendon and tissue health. Adequate nutrition, particularly protein and micronutrients involved in collagen synthesis, supports healing capacity. Regular exercise improves circulation and reduces systemic inflammation. Managing chronic conditions like diabetes prevents complications that increase trigger finger risk.
Individuals with diabetes should work closely with healthcare providers to maintain optimal blood sugar control. Diabetes management resources provide guidance on preventing complications including trigger finger. Those with rheumatoid arthritis benefit from consistent disease management to reduce inflammatory burden on hand structures.
Early Intervention Approach
Recognizing early warning signs—morning stiffness, mild catching, slight pain—enables prompt treatment before significant inflammation develops. Early intervention with conservative measures prevents progression to severe cases requiring surgery. Consulting healthcare providers at symptom onset, rather than waiting for severe dysfunction, optimizes outcomes.
Consider discussing trigger finger prevention with occupational therapists who can assess your specific risk factors and recommend targeted strategies. Finding local therapy services provides access to specialists in hand rehabilitation who offer preventive education.
Frequently Asked Questions
How long does trigger finger take to heal with conservative treatment?
Most patients experience significant improvement within 4-6 weeks of starting conservative treatment combining rest, NSAIDs, splinting, and physical therapy. However, complete resolution may take 8-12 weeks. Some people achieve full recovery in 2-3 weeks with early intervention, while others require longer timeframes. Consistency with prescribed treatments accelerates healing.
Can trigger finger go away on its own without treatment?
Mild cases sometimes resolve spontaneously with activity modification alone, but most cases require active treatment. Waiting without intervention risks symptom progression and development of chronic inflammation. Early treatment prevents complications and typically produces faster resolution than natural healing.
Is surgery always necessary for trigger finger?
No—surgery is reserved for cases where conservative treatment fails or symptoms severely limit function. Approximately 70% of patients achieve adequate relief with non-surgical approaches. Surgery becomes appropriate when symptoms persist 8-12 weeks despite conservative care, or when functional limitations justify surgical intervention.
What exercises should I avoid with trigger finger?
Avoid forceful gripping, heavy lifting, and activities causing pain or locking. Repetitive finger flexion and sustained gripping activities should be minimized during acute phases. As symptoms improve, gradually resume activities under therapist guidance. Pain serves as a guide—activities causing pain should be avoided or modified.
Can trigger finger affect multiple fingers?
Yes, approximately 10% of patients develop trigger finger affecting multiple fingers, often sequentially. This may indicate systemic inflammatory conditions like rheumatoid arthritis requiring broader medical management. Treatment approaches remain similar, though underlying causes may need additional attention.
What is the cost of trigger finger treatment?
Conservative treatment costs vary based on component services. Consultation with healthcare providers, conservative care, and hand therapy represent initial expenses. Injections cost more than conservative care but less than surgery. Understanding therapy cost information helps with planning. Insurance coverage varies significantly—checking your specific policy determines out-of-pocket expenses.
Are there risk factors that increase trigger finger likelihood?
Yes—age over 40, female gender, diabetes, rheumatoid arthritis, and occupations involving repetitive gripping significantly increase risk. Hypothyroidism and carpal tunnel syndrome also correlate with trigger finger development. Understanding your risk factors enables preventive action.
How effective are corticosteroid injections for trigger finger?
Corticosteroid injections provide relief in 50-90% of cases, with success rates highest when performed early and combined with activity modification. Relief typically occurs within 1-2 weeks. However, symptoms may recur in 10-30% of patients within one year, potentially requiring repeat injections or surgery.
What happens after trigger finger surgery?
Recovery from open surgical release typically takes 2-4 weeks, with most patients resuming normal activities within 4-6 weeks. Physical therapy optimizes outcomes and prevents stiffness. Success rates exceed 95%, with most patients experiencing complete symptom resolution and maintained function long-term.
Can I return to work during trigger finger treatment?
This depends on your job and symptom severity. Jobs involving light activity and minimal gripping can often continue with modifications. Jobs requiring heavy gripping or repetitive hand use may require temporary modifications or leave. Discuss work capacity with your healthcare provider and consider consulting occupational therapists for workplace accommodations.


