
How Mindfulness Boosts Mental Health: Expert Insights
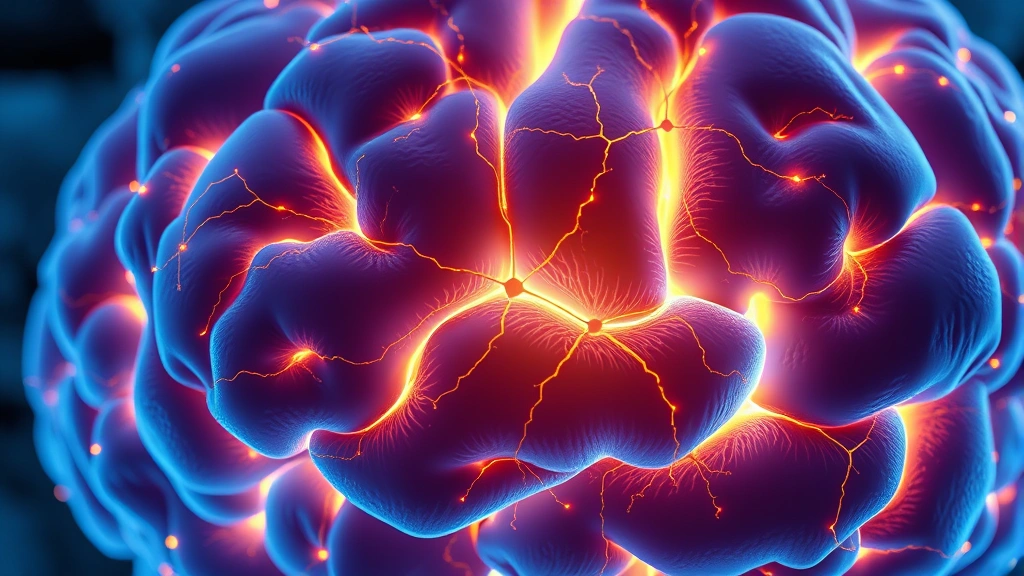
Mindfulness has emerged as one of the most scientifically validated approaches to improving mental health in recent decades. By cultivating present-moment awareness and non-judgmental observation of thoughts and emotions, individuals can fundamentally transform their relationship with stress, anxiety, and depression. This ancient practice, rooted in Buddhist meditation traditions, has been rigorously studied by neuroscientists and psychologists, revealing measurable changes in brain structure and function that correlate with improved psychological well-being.
The integration of mindfulness into mainstream healthcare represents a significant shift in how we approach mental wellness. Rather than relying solely on pharmaceutical interventions, many therapists and counselors now incorporate mindfulness-based techniques into their treatment protocols. Whether you’re exploring options like therapy resources and articles, understanding the insurance coverage for couples therapy, or seeking therapy for teens near you, mindfulness serves as a complementary tool that enhances overall treatment effectiveness.
The Science Behind Mindfulness and Brain Health
Neuroimaging studies have demonstrated that regular mindfulness meditation produces measurable changes in brain regions associated with emotional regulation, self-awareness, and stress response. Research published by Frontiers in Human Neuroscience shows that practitioners experience increased gray matter density in the prefrontal cortex and anterior insula, areas critical for attention control and emotional processing. These structural changes correlate directly with reduced symptoms of anxiety and depression.
The amygdala, often called the brain’s alarm system, shows reduced reactivity in individuals who practice mindfulness regularly. This doesn’t mean practitioners become emotionally numb; rather, they develop the capacity to observe emotional responses without being overwhelmed by them. The anterior cingulate cortex, responsible for attention regulation and emotional control, demonstrates enhanced connectivity in mindfulness practitioners, enabling better management of intrusive thoughts and rumination patterns.
Dr. Jon Kabat-Zinn, founder of Mindfulness-Based Stress Reduction (MBSR), pioneered research demonstrating that eight weeks of mindfulness training produces measurable improvements in immune function and pain perception. His work at the University of Massachusetts Medical School established mindfulness as a legitimate clinical intervention, paving the way for its integration into hospitals and mental health clinics worldwide. The neuroplasticity underlying these changes reveals that our brains remain adaptable throughout life, responding positively to intentional practice.
Mindfulness for Anxiety and Stress Reduction
Anxiety disorders represent one of the most prevalent mental health conditions, affecting millions globally. Traditional treatments often include cognitive-behavioral therapy and medication, but mindfulness offers a complementary approach that addresses the root mechanisms of anxiety. When we practice mindfulness, we interrupt the automatic thought patterns that fuel anxiety spirals, creating space between stimulus and response where choice becomes possible.
The “worry loop” that characterizes anxiety disorders involves repetitive negative thinking about future events. Mindfulness training teaches individuals to observe these thoughts without engaging with them, recognizing them as mental events rather than objective truths. Research from the American Psychological Association indicates that mindfulness-based interventions reduce anxiety symptoms with effectiveness comparable to some pharmaceutical treatments, without the associated side effects.
Breathing exercises form a cornerstone of mindfulness practice for anxiety management. The vagus nerve, which regulates the parasympathetic nervous system, responds directly to breathing patterns. Slow, deliberate breathing activates the relaxation response, counteracting the fight-or-flight activation that characterizes anxiety. Techniques like box breathing (inhaling for four counts, holding for four, exhaling for four, holding for four) provide immediate physiological relief while simultaneously training attention and present-moment awareness.
Generalized anxiety disorder, characterized by persistent worry about multiple life domains, responds particularly well to mindfulness interventions. A study published in JAMA Psychiatry found that mindfulness-based stress reduction produced comparable symptom reduction to pharmaceutical treatment for generalized anxiety, with participants reporting sustained improvements months after completing the program. This suggests that mindfulness develops lasting psychological resources rather than merely masking symptoms.
Depression Management Through Mindful Awareness
Depression often involves rumination—repetitive focus on negative thoughts, past failures, and hopelessness about the future. Mindfulness-Based Cognitive Therapy (MBCT), developed specifically for depression relapse prevention, combines mindfulness meditation with cognitive therapy principles to interrupt rumination patterns. The approach recognizes that depression frequently recurs because individuals fall back into automatic thought patterns during mood fluctuations.
Rather than attempting to replace negative thoughts with positive ones, MBCT teaches practitioners to change their relationship with thoughts themselves. This subtle but crucial distinction addresses the exhaustion many depressed individuals experience when trying to “think positively.” Instead, mindfulness allows people to observe negative thoughts without judgment, recognizing them as temporary mental phenomena rather than accurate reflections of reality. Research demonstrates that this approach reduces depression relapse rates by up to 50% in individuals with recurrent depression.
The anhedonia characteristic of depression—loss of pleasure in previously enjoyed activities—responds to mindfulness through renewed sensory engagement. Mindful eating, mindful walking, and mindful observation of nature activate the sensory systems and present-moment awareness that depression suppresses. By intentionally bringing full attention to everyday experiences, individuals rediscover richness and meaning in activities that had become gray and lifeless.
Neurochemical changes accompanying mindfulness practice support depression recovery. Regular meditation increases serotonin production and enhances dopamine regulation, addressing the neurochemical imbalances underlying depression. Unlike pharmaceutical interventions that work externally on brain chemistry, mindfulness engages the brain’s intrinsic healing mechanisms, fostering genuine neurobiological recovery rather than symptom suppression.
Mindfulness in Therapeutic Settings
Contemporary therapy increasingly incorporates mindfulness techniques regardless of the primary therapeutic modality. Therapists trained in mindfulness bring present-moment awareness and non-judgment into the therapeutic relationship itself, creating a more authentic and healing encounter. This integration proves especially valuable when addressing trauma, where clients often dissociate or become overwhelmed by emotional intensity.
Acceptance and Commitment Therapy (ACT), a modern therapeutic approach, uses mindfulness as a foundational tool for psychological flexibility. Rather than eliminating distressing thoughts and emotions, ACT teaches clients to accept their internal experiences while committing to values-aligned action. This approach proves particularly effective for chronic pain, where suffering often amplifies when individuals struggle against pain rather than accepting its presence while maintaining engagement with meaningful activities.
Understanding how long therapeutic processes take helps set realistic expectations for mental health recovery. Just as physical therapy costs and timelines vary based on individual circumstances, mental health treatment duration depends on condition severity, treatment frequency, and personal commitment. Many clients benefit from understanding physical therapy cost structures and similarly, the investment in regular therapy sessions supporting mindfulness practice.
Group-based mindfulness programs offer cost-effective alternatives to individual therapy while providing community support. MBSR programs, typically eight weeks of weekly classes plus a full-day retreat, cost significantly less than ongoing individual therapy while producing comparable benefits for stress reduction and anxiety. The group format normalizes mental health challenges and combats the isolation many individuals experience.

Practical Mindfulness Techniques for Daily Life
Implementing mindfulness doesn’t require special equipment, dedicated space, or extensive time commitments. Simple techniques integrated into daily routines create cumulative benefits that transform mental health over time. The key involves consistency and gentle persistence rather than perfectionism or intense effort.
Body Scan Meditation: This foundational technique involves systematically directing attention through different body regions, noticing sensations without attempting to change them. Starting at the toes and moving toward the head, practitioners develop interoceptive awareness—the ability to sense internal bodily states. This practice proves especially valuable for individuals disconnected from their bodies due to trauma or chronic stress. Even ten minutes daily produces noticeable improvements in emotional regulation and stress awareness.
Mindful Breathing: Returning attention to the breath serves as an anchor for present-moment awareness. When the mind wanders—as it inevitably does—gently redirecting attention back to breath sensations strengthens attention control. This simple practice can be done anywhere: during work breaks, before important meetings, or when anxiety begins rising. The physiological calming from focused breathing combines with psychological benefits of present-moment awareness.
Loving-Kindness Meditation: This practice cultivates compassion through systematic mental repetition of kind wishes toward oneself and others. Beginning with self-compassion, practitioners extend wishes of well-being toward loved ones, neutral individuals, difficult people, and finally all beings. Research shows this practice reduces negative self-criticism, increases positive emotion, and improves interpersonal relationships. For individuals struggling with depression or low self-worth, loving-kindness meditation provides direct antidote to self-directed hostility.
Mindful Movement: Yoga, tai chi, and walking meditation integrate mindfulness with physical activity. These practices prove particularly valuable for individuals who find sitting meditation difficult. The combination of movement, breath awareness, and present-moment focus produces both physical and mental health benefits. For those interested in understanding how insurance covers physical therapy, mindful movement practices often qualify as part of integrated wellness plans.
Mindful Eating: This technique applies mindfulness to nourishment, bringing full sensory awareness to eating experiences. By slowing down, noticing colors, textures, flavors, and satiety cues, individuals develop healthier relationships with food while simultaneously experiencing greater satisfaction from smaller quantities. This practice addresses both stress-related eating and disconnection from bodily hunger signals common in modern life.
Integrating Mindfulness with Physical Wellness
Mental and physical health remain fundamentally interconnected, with mindfulness serving as a bridge between psychological and physiological well-being. The mind-body connection operates bidirectionally: mental stress produces physical tension and inflammation, while mindful awareness and relaxation practices reduce physical symptoms. This integration proves especially relevant for individuals managing chronic conditions alongside mental health challenges.
The stress response, designed for acute physical threats, becomes pathological when chronically activated by psychological stressors. Mindfulness interrupts this cycle by calming the nervous system and reducing inflammatory markers associated with chronic stress. Individuals practicing mindfulness show lower cortisol levels, reduced inflammation, improved sleep quality, and better immune function—measurable physical health improvements stemming from mental practice.
For individuals recovering from physical injuries or managing chronic pain, mindfulness complements physical rehabilitation. Understanding that physical therapy costs vary based on treatment duration and complexity, individuals benefit from integrating mindfulness to enhance recovery. Mindfulness reduces pain perception not through distraction but through changing the emotional and cognitive relationship with pain sensations, enabling greater participation in rehabilitation exercises.
Sleep quality, fundamental to mental health, improves significantly with mindfulness practice. Body scan meditation, loving-kindness practice, and breathing exercises prepare the nervous system for sleep while addressing the racing thoughts and anxiety that disrupt rest. Research shows mindfulness-based interventions produce sleep improvements comparable to sleep medications without residual grogginess or dependency concerns.
The immune system responds to mindfulness through multiple pathways: reduced stress hormones, decreased inflammation, improved sleep, and enhanced parasympathetic activation all strengthen immune function. Regular meditators show increased antibody production and improved response to vaccines, suggesting mindfulness produces tangible immunological benefits. This mind-body integration demonstrates that mental health practices produce real physiological consequences.
FAQ
How long does it take to experience mindfulness benefits?
Many individuals notice immediate calming effects from single mindfulness sessions, with anxiety reduction and improved focus appearing within minutes. However, sustained neurobiological changes and lasting symptom improvement typically emerge after four to eight weeks of consistent practice. The research establishing MBSR’s effectiveness used eight-week programs, though benefits continue accumulating with longer-term practice. Consistency matters more than duration—daily ten-minute practice produces better results than sporadic hour-long sessions.
Can mindfulness replace medication for mental health conditions?
Mindfulness serves as a valuable complement to psychiatric medication rather than a replacement. For many individuals, combining mindfulness with medication produces better outcomes than either approach alone. Medication manages acute symptoms while mindfulness develops lasting psychological resources and addresses root causes. Individuals considering medication changes should consult psychiatrists rather than making unilateral decisions. Mindfulness proves particularly valuable during medication tapering, helping individuals develop coping skills as pharmaceutical support decreases.
What’s the difference between mindfulness and meditation?
Meditation refers to specific formal practices like sitting quietly and focusing attention, while mindfulness represents a broader quality of present-moment awareness applicable to any activity. All meditation practices develop mindfulness, but mindfulness extends beyond formal meditation into daily life—mindful eating, walking, and conversation. Individuals resistant to formal meditation can develop mindfulness through movement practices, mindful activity, and deliberate present-moment attention during routine tasks.
Does mindfulness work for everyone?
Research demonstrates mindfulness produces benefits across diverse populations, though individual responses vary. Some people experience dramatic improvements while others notice subtle shifts. Trauma survivors sometimes find sitting meditation triggering, requiring modified approaches like movement-based mindfulness. Cultural backgrounds influence comfort with meditation practices, making it valuable to explore diverse mindfulness traditions. Working with qualified teachers helps individuals find approaches matching their temperament and circumstances.
How does mindfulness differ from relaxation techniques?
While mindfulness and relaxation both calm the nervous system, they operate differently. Relaxation aims to achieve a calm state through muscles relaxation and breathing techniques. Mindfulness emphasizes awareness and observation rather than achieving particular states. In fact, mindfulness accepts whatever arises—calm, agitation, or neutral sensation—without judgment. This distinction proves important because individuals seeking relaxation for anxiety sometimes become frustrated if mindfulness doesn’t produce expected calm, not recognizing that accepting restlessness without struggle produces psychological freedom.



