
Negative Pressure Therapy: Expert Insights & Benefits
Negative pressure wound therapy (NPWT) represents one of the most significant advances in modern wound care management. Also known as vacuum-assisted closure therapy, this innovative treatment modality has transformed how healthcare providers approach chronic and acute wounds across diverse clinical settings. Whether you’re a patient seeking effective wound treatment options in Palm Coast or a healthcare professional looking to understand the latest therapeutic approaches, negative pressure therapy offers compelling evidence-based benefits backed by decades of clinical research.
The technology works by applying controlled subatmospheric pressure to wound surfaces, creating an environment that actively promotes healing while simultaneously removing excess fluid and infectious material. This mechanism has proven particularly effective for complex wounds that have traditionally resisted conventional treatment methods. Understanding how negative pressure wound therapy functions and its applications can help patients and clinicians make informed decisions about wound care strategies.
How Negative Pressure Therapy Works
Negative pressure wound therapy operates through a sophisticated yet elegant mechanism that harnesses physics to accelerate the body’s natural healing response. The system consists of a sealed dressing connected to a pump that generates controlled subatmospheric pressure, typically ranging from 50 to 175 millimeters of mercury below atmospheric pressure. This vacuum environment initiates multiple physiological cascades that work synergistically to promote wound closure and tissue regeneration.
When negative pressure is applied to a wound, several critical processes occur simultaneously. First, the system removes excess interstitial fluid, exudate, and potentially contaminated material from the wound bed. This drainage mechanism alone significantly reduces bacterial colonization and creates a cleaner environment conducive to healing. The removal of wound fluid also reduces edema in surrounding tissues, improving microcirculation and oxygen delivery to the injured area—a crucial factor in tissue repair.
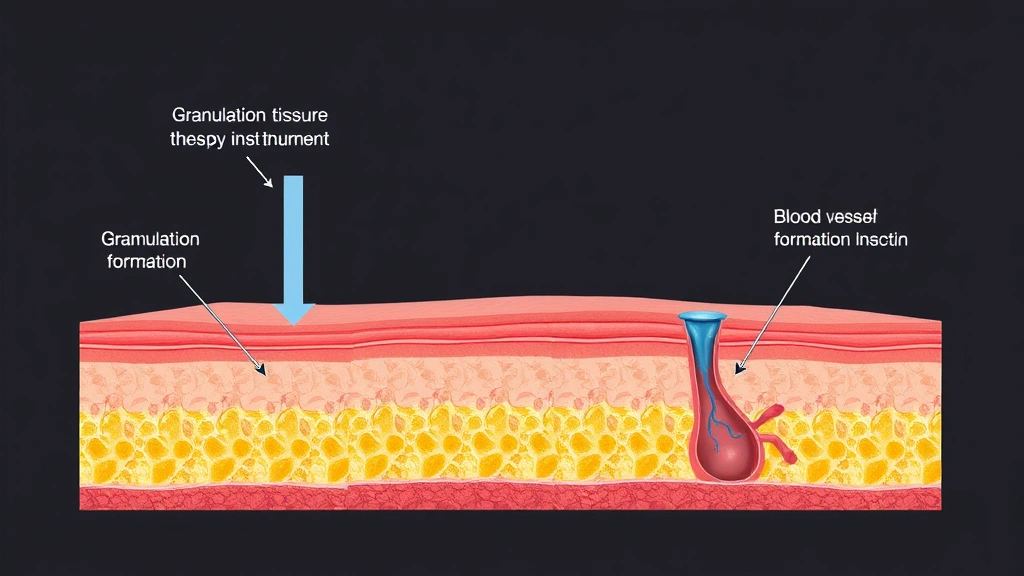
Beyond fluid removal, the negative pressure directly stimulates cellular responses at the molecular level. Research demonstrates that NPWT increases angiogenesis, the formation of new blood vessels essential for delivering nutrients and oxygen to healing tissues. Additionally, the therapy promotes fibroblast proliferation and collagen deposition, the foundational proteins necessary for strong tissue regeneration. The mechanical forces generated by the negative pressure also encourage cell migration and proliferation, essentially accelerating the wound’s natural progression through healing phases.
The dressing systems used in negative pressure therapy have evolved considerably. Modern systems employ either open-cell or closed-cell foam inserts that distribute pressure evenly across the wound surface. Some advanced systems incorporate instillation therapy, which periodically delivers antimicrobial or nutritive solutions into the wound, further enhancing the therapeutic environment. These technological refinements have made NPWT increasingly effective and adaptable to various wound types and anatomical locations.
Clinical Applications and Conditions Treated
Negative pressure wound therapy has proven remarkably versatile, with applications extending across numerous medical specialties and wound classifications. Originally developed for managing traumatic injuries and surgical complications, NPWT now represents a standard treatment option for diverse wound etiologies. Understanding which conditions benefit most from this therapy helps clinicians and patients appreciate its broad clinical utility.
Chronic wounds represent one of the primary applications for negative pressure therapy. Diabetic foot ulcers, which affect millions of individuals globally, respond exceptionally well to NPWT. These notoriously difficult-to-heal wounds often involve compromised circulation and impaired inflammatory responses, making them resistant to conventional dressings. The active healing environment created by negative pressure therapy significantly improves healing rates for diabetic wounds requiring specialized wound care approaches. Similarly, pressure ulcers (bedsores) that develop in immobilized patients frequently benefit from NPWT, which addresses both the mechanical and biological factors contributing to their development.
Venous leg ulcers, caused by venous insufficiency, also respond favorably to negative pressure therapy when combined with compression therapy. The improved circulation and reduced edema from NPWT complement compression strategies, creating a comprehensive approach to venous wound management. Burns represent another significant application area, particularly for deep partial-thickness and full-thickness injuries where conventional treatment might require extensive skin grafting.
Post-surgical complications provide another important indication for NPWT. Surgical site infections, dehiscence (wound separation), and other post-operative complications can be effectively managed with negative pressure therapy, often preventing the need for additional surgical interventions. Acute traumatic wounds, including those from motor vehicle accidents or penetrating injuries, frequently benefit from NPWT’s ability to manage contamination and promote rapid healing. For patients in Palm Coast seeking comprehensive wound care solutions, NPWT availability represents an important therapeutic option.

Benefits of NPWT Treatment
The evidence supporting negative pressure wound therapy continues to accumulate through rigorous clinical research and real-world outcomes. Patients and healthcare providers recognize multiple compelling benefits that distinguish NPWT from conventional wound care approaches. These advantages extend beyond simple wound closure to encompass broader health outcomes and quality of life improvements.
Accelerated healing represents the most obvious benefit of negative pressure therapy. Clinical studies consistently demonstrate that NPWT reduces time to wound closure compared to standard dressing approaches. For chronic wounds that might require months of conventional treatment, NPWT can reduce healing timelines by 30-50 percent or more. This acceleration carries profound implications for patient morbidity, functional recovery, and healthcare costs. Faster wound closure means reduced infection risk, shorter hospitalization periods, and faster return to normal activities.
Infection reduction constitutes another critical advantage. The negative pressure environment actively inhibits bacterial proliferation while the continuous fluid removal eliminates bacterial growth substrates. This combination creates a hostile environment for pathogenic organisms while promoting the growth of beneficial granulation tissue. For patients with contaminated or infected wounds, NPWT often enables successful treatment without requiring systemic antibiotics or additional surgical debridement.
Improved tissue quality represents a less obvious but equally important benefit. Wounds treated with negative pressure therapy develop more robust, vascularized granulation tissue compared to conventional dressing treatments. This superior tissue quality not only promotes better healing but also creates stronger scar tissue less prone to re-ulceration. For chronic wound patients at high risk of recurrence, this tissue quality improvement translates to long-term functional benefits.
Patient comfort and convenience have improved significantly with modern NPWT systems. Unlike older, bulky equipment, contemporary negative pressure devices are portable, allowing patients to maintain mobility and independence during treatment. Some systems operate quietly and discreetly, enabling patients to continue working and engaging in social activities. These practical advantages enhance compliance and patient satisfaction with therapy.
Reduced need for surgical intervention represents another substantial benefit, particularly for complex wounds. By promoting healing in wounds that might otherwise require skin grafting or surgical reconstruction, NPWT can avoid the morbidity and costs associated with surgical procedures. This benefit extends to trauma patients, surgical patients, and those with chronic wounds who might otherwise face amputation risk.
Finding Negative Pressure Therapy in Palm Coast
Patients in Palm Coast seeking negative pressure wound therapy have access to several healthcare delivery options. Understanding where to find this specialized treatment and what to expect from the process helps ensure successful therapeutic outcomes. The availability of NPWT has expanded significantly, with multiple healthcare settings now offering this technology.
Hospital wound care centers represent primary sources for negative pressure therapy in Palm Coast. These facilities maintain comprehensive wound care programs staffed by specialized physicians, nurses, and technicians trained in NPWT application and management. Hospital-based programs typically handle complex cases requiring intensive monitoring or those complicated by systemic disease. The multidisciplinary approach available in hospital settings ensures comprehensive wound management addressing underlying conditions contributing to poor healing.
Outpatient wound clinics have proliferated throughout Florida, including the Palm Coast area. These specialized facilities focus exclusively on wound management, offering NPWT along with other advanced therapies. Outpatient clinics provide convenient access for patients with chronic wounds who don’t require hospitalization. Many outpatient programs coordinate care with comprehensive therapy resources and rehabilitation services to address factors contributing to wound development.
Home healthcare agencies in Palm Coast increasingly provide negative pressure therapy in home settings. For appropriate candidates, home-based NPWT offers maximum convenience and comfort while maintaining clinical efficacy. Home programs require careful patient selection and reliable patient compliance but provide exceptional quality-of-life benefits for suitable patients. Skilled nursing visits ensure proper dressing changes and system monitoring while allowing patients to recover in their own environments.
Selecting an appropriate provider involves evaluating several factors. Verify that providers hold appropriate credentials and certifications in wound care management. Ask about the specific NPWT systems they utilize, as different systems offer varying features and capabilities. Inquire about their experience managing your particular wound type. Understanding their approach to adjunctive therapies—such as compression for venous wounds or glycemic control for diabetic wounds—ensures comprehensive treatment addressing underlying causes.
Recovery and Patient Outcomes
Understanding typical recovery trajectories and expected outcomes helps patients develop realistic expectations and maintain motivation during treatment. Negative pressure therapy outcomes vary based on wound characteristics, patient factors, and treatment compliance, but overall results demonstrate remarkable success rates across diverse populations.
Initial response to negative pressure therapy typically becomes evident within the first one to two weeks of treatment. Patients often notice reduced wound odor, decreased drainage, and improved surrounding skin condition. These early improvements reflect the therapy’s effectiveness in removing contaminated fluid and creating a healing environment. Pain often decreases as well, contributing to improved patient comfort and quality of life.
Granulation tissue development represents a key milestone in the healing process. As negative pressure therapy continues, patients and clinicians observe the progressive development of healthy, red, vascularized granulation tissue replacing necrotic or infected material. This tissue transformation indicates the wound is progressing through appropriate healing phases. The timeline for granulation tissue development varies but typically accelerates compared to conventional treatment.
Wound size reduction follows predictable patterns for responsive wounds. Most wounds treated with NPWT show measurable size reduction within two to four weeks, with continued progressive closure over subsequent weeks or months depending on initial wound size and complexity. Some studies report average healing rates of 1-3 centimeters per week, though individual variation exists. Tracking wound measurements and photographing wounds provides objective documentation of progress.
Complete wound closure timelines depend on initial wound characteristics. Small acute wounds might achieve closure within weeks, while large chronic wounds might require months of therapy. Most studies report that 60-80 percent of appropriately selected wounds achieve complete closure with negative pressure therapy, either as monotherapy or combined with other interventions. Wounds failing to progress may require reassessment of underlying factors or adjustment of treatment parameters.
Long-term outcomes focus on wound recurrence and functional recovery. Patients who achieve wound closure through negative pressure therapy and subsequently address underlying contributing factors (such as improved glycemic control, compression therapy compliance, or pressure relief strategies) demonstrate low recurrence rates. This long-term success reflects the durable tissue quality improvements resulting from NPWT treatment.
Cost Considerations and Insurance
Understanding the financial aspects of negative pressure therapy helps patients plan for treatment and navigate insurance coverage. While NPWT involves significant costs, the investment often proves economical when considering reduced hospitalization, prevented complications, and accelerated healing compared to conventional approaches.
Equipment costs represent the primary expense component. Negative pressure systems range from several hundred to several thousand dollars, depending on device sophistication and features. Most patients don’t purchase systems outright but rather rent or receive them through insurance coverage. Dressing supplies, including foam inserts and adhesive drapes, require regular replacement throughout treatment. These consumable costs accumulate but remain substantially less than extended hospitalization or surgical interventions.
Insurance coverage for negative pressure therapy has expanded considerably as evidence of efficacy continues accumulating. Medicare generally covers NPWT for appropriate wound indications when prescribed by qualified physicians. Specific coverage criteria require documentation of wound characteristics, failed conventional treatment attempts, and medical necessity. Private insurance plans typically follow similar coverage patterns, though specific requirements vary by plan.
For patients seeking detailed information about therapy costs and insurance coverage, direct communication with providers and insurance companies proves essential. Many wound care centers maintain insurance specialists who navigate coverage complexities and maximize benefits for patients. Understanding out-of-pocket costs, deductibles, and co-insurance obligations allows patients to plan financially for treatment.
Medicaid coverage varies by state and program, with Florida’s Medicaid program generally supporting NPWT for appropriate indications. Veterans receiving care through VA facilities often have excellent access to negative pressure therapy with minimal out-of-pocket costs. Uninsured patients should inquire about payment plans or financial assistance programs available through treatment facilities.
Comparative cost analysis demonstrates NPWT’s economic value despite initial expenses. A single surgical debridement procedure costs $1,500-3,000, while extended hospitalization for infected wounds can easily exceed $10,000-20,000. The prevention of such complications through early NPWT intervention frequently results in net cost savings despite therapy expenses. Additionally, accelerated healing reduces lost work productivity and caregiver burden, creating economic benefits extending beyond direct medical costs.
Frequently Asked Questions
What exactly is negative pressure wound therapy?
Negative pressure wound therapy uses controlled subatmospheric pressure applied through sealed dressings to promote wound healing. The system removes excess fluid, reduces infection risk, and stimulates the body’s natural healing processes through mechanical and biological mechanisms. It’s particularly effective for chronic and complex wounds resistant to conventional treatment.
How long does negative pressure therapy treatment typically last?
Treatment duration varies widely based on wound size, depth, and type. Small acute wounds might require weeks of therapy, while large chronic wounds may require months. Most patients undergo treatment for 4-12 weeks on average, though individual timelines vary considerably. Healthcare providers establish specific treatment goals and monitor progress regularly.
Is negative pressure therapy painful?
Most patients tolerate NPWT well with minimal pain. Initial dressing application might cause mild discomfort, but once the system is functioning, pain typically decreases compared to conventional dressing changes. Some patients report improved comfort as wound healing progresses and reduces wound-related pain. Pain management can be optimized through medication timing and provider communication.
Can negative pressure therapy be used at home?
Yes, appropriate candidates can receive NPWT in home settings through home healthcare agencies. Home-based therapy offers convenience and comfort advantages while maintaining clinical efficacy. Home programs require reliable patients with support systems and access to professional monitoring. Healthcare providers assess suitability for home therapy based on wound characteristics and patient factors.
What are the main contraindications for negative pressure therapy?
Absolute contraindications include exposed blood vessels, organs, or bone without protective tissue coverage, and untreated osteomyelitis. Relative contraindications include active bleeding, malignancy in the wound, and certain medications affecting healing. Individual assessment by qualified healthcare providers determines appropriateness for specific patients.
How does negative pressure therapy compare to skin grafting?
NPWT often enables wound closure without requiring surgical skin grafting procedures. For appropriate wounds, NPWT generates sufficient granulation tissue and healing to achieve closure through secondary intention or with minimal grafting. This approach avoids surgical morbidity, donor site complications, and extended recovery periods associated with grafting while producing comparable or superior functional outcomes.
Will my insurance cover negative pressure therapy in Palm Coast?
Most insurance plans, including Medicare and private insurers, cover NPWT for appropriate indications when prescribed by qualified physicians. Coverage requires documentation of medical necessity and typically evidence of failed conventional treatment. Contacting your insurance provider and treatment facility’s insurance specialists clarifies specific coverage for your situation.
What should I expect during NPWT treatment?
Initial treatment involves wound assessment, cleansing, and dressing application by trained professionals. Subsequent visits typically occur 2-3 times weekly for dressing changes and wound monitoring. Patients notice progressive improvements in wound appearance, reduced odor and drainage, and decreased pain. Regular measurements and photographs document healing progress objectively.



