
Is Craniosacral Therapy Effective? Expert Insights on Craniosacral Fascial Therapy
Craniosacral therapy has gained significant popularity in wellness circles over the past two decades, with practitioners and patients alike claiming remarkable benefits for pain relief, stress reduction, and overall health optimization. Yet despite its widespread adoption, the scientific community remains divided on whether this gentle manual therapy delivers measurable therapeutic outcomes or operates primarily through placebo effects. Understanding the evidence behind craniosacral fascial therapy requires examining both rigorous clinical research and the theoretical mechanisms that practitioners propose.
This comprehensive guide explores the current state of evidence for craniosacral therapy, examining what peer-reviewed studies reveal about its effectiveness, how it compares to other therapeutic modalities like physical therapy in Los Angeles, and what experts recommend for patients considering this treatment option. Whether you’re a healthcare provider seeking evidence-based information or a patient evaluating your treatment options, this analysis provides the critical insights needed to make informed decisions.
Understanding Craniosacral Therapy and Fascial Release
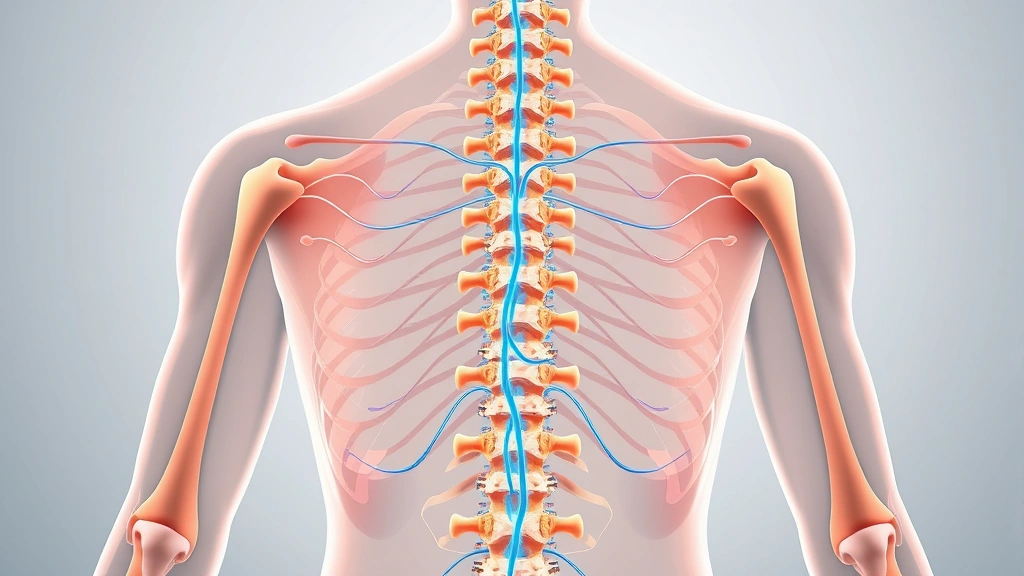
Craniosacral therapy emerged in the 1970s when osteopathic physician John Upledger developed and systematized techniques based on earlier osteopathic concepts. The therapy operates on the premise that restrictions in the craniosacral system—comprising the brain, spinal cord, cerebrospinal fluid, meninges, and associated fascial tissues—can impair overall health and function. Practitioners use gentle manual techniques to palpate what they describe as the “craniosacral rhythm,” a subtle rhythmic motion they believe reflects cerebrospinal fluid movement and fascial mobility.
The craniosacral fascial therapy approach integrates concepts from fascial research, emphasizing the interconnected network of connective tissue throughout the body. Fascia, the continuous web of connective tissue surrounding muscles, organs, and nerves, has become increasingly recognized as physiologically significant. Recent research from institutions like the Karolinska Institute has demonstrated that fascia contains proprioceptors and nociceptors, suggesting it plays a more active role in sensory perception and pain modulation than previously understood. However, whether craniosacral techniques specifically influence fascia in therapeutically meaningful ways remains contested.
Traditional craniosacral therapy differs from other manual therapies in its specificity and gentleness. Rather than aggressive soft tissue mobilization, practitioners apply pressure typically measured in grams—roughly equivalent to the weight of a coin—to specific anatomical locations. This minimalist approach contrasts sharply with deeper manual techniques used in physical therapy practices and myofascial release methods. The theoretical mechanism involves releasing fascial restrictions, improving cerebrospinal fluid circulation, and facilitating the body’s inherent healing capacity.
The Scientific Evidence Behind Craniosacral Fascial Therapy
The scientific evidence for craniosacral therapy presents a complex picture that demands careful interpretation. A systematic review published in the International Journal of Therapeutic Massage & Bodywork identified numerous studies examining craniosacral therapy’s effects, but quality varied considerably. While some investigations reported positive outcomes for conditions ranging from migraines to fibromyalgia, methodological limitations frequently compromised their reliability. Many studies lacked adequate control groups, employed small sample sizes, or failed to account for placebo effects—critical flaws that undermine confidence in reported benefits.
One significant challenge in craniosacral therapy research involves establishing appropriate control conditions. Unlike pharmaceutical studies where placebo pills provide convincing controls, designing credible sham manual therapy proves difficult. Patients and practitioners often recognize whether they’re receiving actual craniosacral techniques or control interventions, potentially biasing results. Several well-designed trials using rigorous blinding procedures have found that craniosacral therapy performs no better than sham treatment, suggesting that observed improvements may reflect placebo responses rather than specific therapeutic mechanisms.
Research from Cochrane Collaboration, the gold standard for systematic evidence review, has expressed skepticism about craniosacral therapy’s efficacy. Their analyses consistently conclude that evidence remains insufficient to support widespread clinical recommendations, though they acknowledge that additional high-quality research might alter this assessment. The lack of convincing mechanistic explanations compounds these concerns—while practitioners describe palpating craniosacral rhythms, multiple studies using objective measurement devices have failed to validate the existence of this proposed rhythm at claimed frequencies.
Despite these limitations, some research suggests potential benefits for specific populations. Studies examining craniosacral therapy for temporomandibular joint disorders, migraine headaches, and certain pain conditions have occasionally demonstrated statistical improvements compared to controls. However, effect sizes typically remain modest, and clinical significance often remains unclear. Additionally, many positive studies emanate from institutions or researchers with direct financial interests in promoting craniosacral therapy, raising potential bias concerns.
Clinical Applications and Patient Outcomes
In clinical practice, craniosacral fascial therapy practitioners treat an expansive range of conditions, from musculoskeletal pain to neurological disorders. Common applications include chronic headaches and migraines, neck and back pain, fibromyalgia, post-concussion syndrome, temporomandibular joint dysfunction, and stress-related conditions. Some practitioners claim effectiveness for autism spectrum disorders, cerebral palsy, and other developmental conditions—assertions that have attracted particular scrutiny from medical authorities due to vulnerability of affected populations and limited evidence base.
Patient testimonials frequently emphasize subjective improvements in pain, relaxation, and overall wellbeing following craniosacral therapy sessions. These reports merit consideration but require cautious interpretation. Subjective symptom improvement can reflect numerous factors beyond specific treatment effects, including natural disease progression, regression to the mean, concurrent treatments, placebo responses, and therapeutic attention. The power of expectation and the therapeutic relationship in producing symptom relief represents a well-established phenomenon in medicine, sometimes accounting for 30-60% of improvement in pain conditions.
Comparing outcomes across patient populations reveals inconsistent results. Some individuals report dramatic symptom resolution after craniosacral therapy, while others experience minimal benefit despite multiple sessions. This variability makes predicting individual treatment responses challenging. Patients considering craniosacral therapy should understand that outcomes remain unpredictable, and evidence supporting its use for most conditions remains limited compared to established therapies like cognitive behavioral therapy for anxiety disorders or evidence-based physical rehabilitation.
For patients with stress-related symptoms or those seeking gentle therapeutic touch, craniosacral therapy may provide value through mechanisms including relaxation response activation, parasympathetic nervous system engagement, and therapeutic attention. However, distinguishing these nonspecific therapeutic benefits from effects specific to craniosacral techniques remains scientifically difficult. Patients might achieve similar relaxation benefits through other gentle modalities, meditation, or therapeutic massage.
How Craniosacral Therapy Compares to Conventional Treatments
When evaluating craniosacral therapy’s place in the therapeutic landscape, comparison with established evidence-based treatments provides important context. For chronic pain conditions, substantial evidence supports physical therapy approaches involving exercise, movement retraining, and progressive loading. These interventions demonstrate consistent, measurable improvements in function and pain reduction across numerous high-quality trials. Similarly, for headache disorders, both preventive medications and cognitive-behavioral interventions show robust evidence for efficacy.
Craniosacral therapy’s gentle nature offers one potential advantage: minimal risk of adverse effects. Unlike some interventions, the risk of harm from craniosacral manipulation appears negligible for most patients. This safety profile may appeal to individuals concerned about medication side effects or more aggressive manual techniques. However, safety alone doesn’t establish efficacy—a treatment can be completely harmless while providing no specific therapeutic benefit.
The time and financial investment required for craniosacral therapy deserves consideration. Treatment typically involves multiple sessions at significant cost, often not covered by insurance. Patients investing in craniosacral therapy might alternatively pursue established therapies with stronger evidence bases, such as exercise-based physical rehabilitation, psychological interventions, or other modalities with demonstrated effectiveness. The opportunity cost of delaying or avoiding evidence-based treatments represents a genuine concern, particularly for serious conditions where timely intervention matters.
Some patients find value in combining craniosacral therapy with conventional treatments. For individuals managing stress and seeking complementary relaxation approaches alongside primary medical care, incorporating craniosacral sessions might enhance overall wellbeing. However, craniosacral therapy should never replace evidence-based medical treatment for serious conditions. Integration into comprehensive care requires clear communication between all providers and realistic expectations about each modality’s role.

Expert Perspectives and Professional Recommendations
Medical organizations generally maintain cautious positions regarding craniosacral therapy. The American Physical Therapy Association, while acknowledging practitioners’ interest in craniosacral approaches, emphasizes that evidence remains insufficient to support it as a primary treatment for most conditions. Major medical institutions rarely recommend craniosacral therapy as first-line treatment, instead categorizing it as a complementary or alternative approach suitable only when evidence-based options have been optimized.
Osteopathic physicians, who have historical connections to craniosacral therapy’s development, hold varied perspectives. Some osteopaths enthusiastically practice craniosacral techniques, while others focus on evidence-based osteopathic manipulation or abandon manual techniques entirely in favor of conventional medical practice. This professional diversity reflects broader uncertainty within the field about craniosacral therapy’s scientific standing.
Fascia researchers have contributed important insights without necessarily validating craniosacral therapy specifically. While confirming that fascia contains sensory receptors and participates in proprioception and pain modulation, this research doesn’t necessarily support claims that gentle manual techniques can meaningfully influence fascial function in therapeutically significant ways. The distinction between fascia being physiologically important and craniosacral techniques effectively manipulating fascia remains crucial but often blurred in marketing materials.
Integrative medicine practitioners frequently recommend craniosacral therapy as part of holistic wellness approaches. This perspective values patient experience and symptom improvement alongside scientific evidence, sometimes prioritizing therapeutic relationship and individualized care over randomized controlled trial outcomes. While this approach resonates with many patients, it can sometimes lead to recommending treatments with limited evidence bases, potentially delaying more effective interventions.
Safety Considerations and Contraindications
Craniosacral therapy’s safety profile remains one of its strongest attributes. Adverse events directly attributable to craniosacral manipulation appear exceptionally rare, likely due to the technique’s gentleness and low mechanical force. Unlike spinal manipulation, which carries documented risks including vertebral artery dissection, craniosacral therapy hasn’t generated similar safety concerns. This benign safety profile makes it suitable for fragile populations including elderly individuals, children, and those with multiple comorbidities.
However, certain situations warrant caution or contraindication. Patients with increased intracranial pressure, recent head trauma, or undiagnosed neurological conditions should consult physicians before pursuing craniosacral therapy. Additionally, craniosacral therapy should never delay or substitute for necessary medical evaluation of concerning symptoms. Individuals experiencing acute neurological changes, severe headaches, or unexplained neurological symptoms require proper medical investigation before considering complementary therapies.
The gentle nature of craniosacral therapy shouldn’t create false reassurance about its universal appropriateness. While unlikely to cause direct harm, recommending craniosacral therapy for serious conditions as an alternative to evidence-based treatment represents an indirect harm by delaying appropriate care. Healthcare providers recommending craniosacral therapy bear responsibility for ensuring patients don’t forego necessary conventional treatment based on unrealistic expectations about craniosacral therapy’s effectiveness.
Integrating Craniosacral Therapy Into Comprehensive Care
For patients interested in craniosacral therapy, integration into comprehensive care plans requires thoughtful consideration. Rather than viewing craniosacral therapy as a replacement for evidence-based medicine, some patients find value incorporating it alongside proven treatments. This approach might involve maintaining physical therapy or exercise programs while adding craniosacral sessions for relaxation and stress management.
Clear communication with all healthcare providers becomes essential when integrating multiple modalities. Physicians, physical therapists, and craniosacral practitioners should understand each other’s approaches and coordinate care appropriately. This transparency prevents dangerous interactions, eliminates redundant treatments, and ensures patients receive consistent guidance about their condition and prognosis.
Patients should realistically assess their treatment goals and expectations. If seeking specific pain relief or functional improvement, evidence-based physical therapy or medical treatments typically offer superior track records. If seeking stress reduction, relaxation, and therapeutic attention, craniosacral therapy might provide subjective benefits, though other modalities like massage therapy, meditation, or red light therapy and other complementary approaches might offer similar value at lower cost.
For individuals with anxiety or stress-related conditions, combining evidence-based psychological interventions with complementary relaxation therapies can create synergistic benefits. Patients undergoing couples therapy or other psychological treatment might supplement these approaches with craniosacral sessions as part of holistic self-care. However, psychological interventions with established efficacy should remain primary, with complementary modalities playing supporting roles.
Practitioner selection matters significantly when pursuing craniosacral therapy. Qualified practitioners complete extensive training programs and often maintain professional credentials. However, licensing and regulation vary considerably by jurisdiction. Patients should verify practitioners’ qualifications, ask about their training background, and understand their claims about what craniosacral therapy can accomplish. Practitioners making extraordinary claims about treating serious diseases or replacing medical care warrant particular skepticism.
Frequently Asked Questions
Is craniosacral therapy backed by scientific research?
Scientific evidence for craniosacral therapy remains limited and mixed. While some studies report positive outcomes, many possess significant methodological limitations. Rigorous trials using appropriate control conditions often fail to demonstrate benefits beyond placebo effects. Major medical organizations conclude that evidence remains insufficient to recommend craniosacral therapy as a primary treatment for most conditions.
Can craniosacral therapy treat serious medical conditions?
Craniosacral therapy should not replace evidence-based medical treatment for serious conditions. While some practitioners claim effectiveness for conditions ranging from autism to cerebral palsy, these claims lack strong scientific support. Patients with serious medical conditions require proper medical evaluation and evidence-based treatment as primary approaches.
Is craniosacral therapy safe?
Craniosacral therapy appears exceptionally safe with minimal documented adverse effects. Its gentle nature and low mechanical force make it suitable for fragile populations. However, safety doesn’t establish efficacy. Additionally, recommending craniosacral therapy as an alternative to necessary medical care can indirectly cause harm by delaying appropriate treatment.
How much does craniosacral therapy cost?
Craniosacral therapy typically costs $75-$200 per session, varying by location and practitioner experience. Most insurance plans don’t cover craniosacral therapy, making it an out-of-pocket expense. Patients should consider the financial investment relative to evidence-based alternatives when making treatment decisions.
How many sessions of craniosacral therapy are typically needed?
Treatment duration varies considerably depending on the condition and individual response. Some practitioners recommend series of sessions ranging from 6-12 treatments, while others suggest ongoing periodic sessions. Clear discussion about expected treatment duration and anticipated outcomes should occur before beginning treatment.
Can craniosacral therapy be combined with other treatments?
Yes, craniosacral therapy can complement other treatments when integrated thoughtfully into comprehensive care plans. However, all providers should coordinate care and understand each modality’s role. Craniosacral therapy should supplement rather than replace evidence-based primary treatments.
What is the craniosacral rhythm?
Practitioners describe the craniosacral rhythm as a subtle pulsation reflecting cerebrospinal fluid movement and fascial mobility. However, objective measurement studies have failed to validate this rhythm at claimed frequencies, raising questions about whether practitioners accurately perceive distinct physiological phenomena or interpret subtle sensations through theoretical frameworks.
How does craniosacral therapy compare to massage therapy?
Craniosacral therapy uses gentler pressure and focuses on specific anatomical structures and theoretical mechanisms, while massage therapy employs variable pressure techniques targeting muscle and soft tissue relaxation. Both offer minimal evidence for specific therapeutic effects beyond relaxation and placebo responses, though patient preferences for treatment approach may vary.
The evidence regarding craniosacral fascial therapy suggests a nuanced picture: while the therapy appears safe and some patients report subjective improvements, scientific evidence supporting its efficacy remains limited. Craniosacral therapy may provide value through relaxation, therapeutic attention, and placebo mechanisms, but should not replace evidence-based medical treatment. Patients considering craniosacral therapy should maintain realistic expectations, integrate it thoughtfully into comprehensive care plans, and prioritize established therapies with stronger evidence bases for serious medical conditions. Consulting with qualified healthcare providers about appropriate roles for craniosacral therapy within individual treatment plans remains essential for optimizing outcomes and preventing harm from delayed evidence-based care.


