
Spinal Decompression: Does It Aid Mental Well-being?
The connection between physical pain and mental health has long been established in medical research. When chronic spinal pain affects your daily life, it doesn’t just impact your body—it significantly influences your psychological well-being, mood, and overall quality of life. Spinal decompression therapy has emerged as a promising non-surgical treatment option for those suffering from herniated discs, degenerative disc disease, and chronic back pain. But beyond addressing the physical symptoms, many patients report improvements in their mental health and emotional state after undergoing this treatment.
Understanding whether spinal decompression therapy near me can genuinely aid mental well-being requires examining both the physiological mechanisms and the psychological benefits reported by patients. This comprehensive guide explores the science behind spinal decompression, its impact on pain management, and how relief from chronic pain translates into improved mental health outcomes.
What Is Spinal Decompression Therapy?
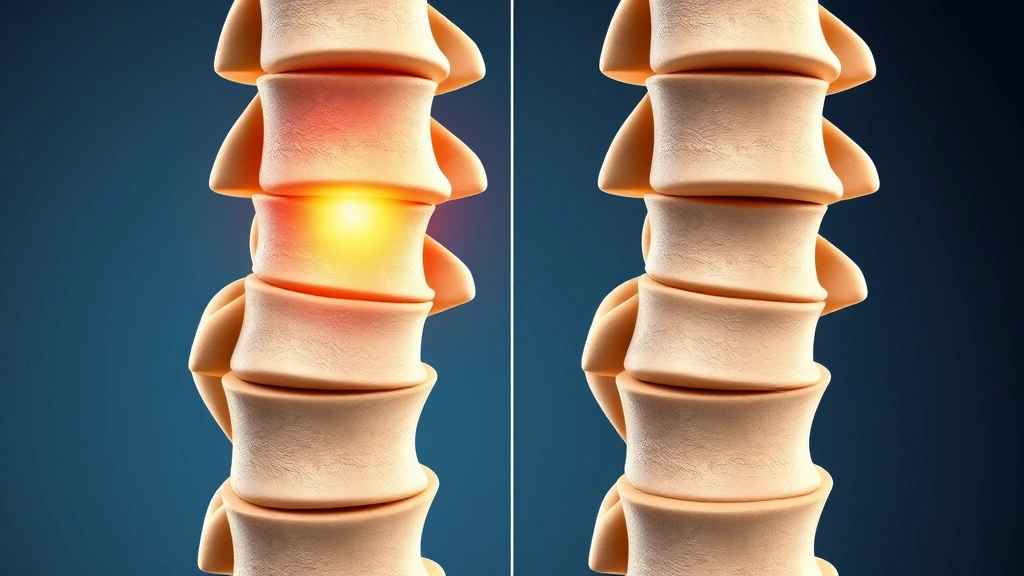
Spinal decompression therapy is a non-invasive treatment designed to relieve pressure on spinal nerves and discs. The procedure typically involves using specialized equipment that gently stretches the spine, creating negative pressure within the intervertebral discs. This negative pressure can help retract herniated disc material and promote nutrient-rich fluid flow to damaged discs, facilitating natural healing processes.
The therapy comes in two main forms: mechanical traction devices and motorized decompression systems. During a typical session, patients lie on a specialized table while the equipment applies controlled tension to specific spinal segments. Treatment sessions usually last 25-45 minutes and are often recommended in series of 15-30 sessions over several weeks. Unlike surgical interventions, spinal decompression offers a conservative approach to managing spinal conditions, making it an attractive option for patients seeking to avoid surgery or medication dependency.
When exploring physical therapy treatment options, many healthcare providers recommend spinal decompression as part of a comprehensive pain management strategy. The procedure has gained significant attention from both patients and clinicians as a bridge between conservative care and surgical intervention.
The Pain-Mental Health Connection
Chronic pain and mental health are intrinsically linked through multiple biological and psychological pathways. When your body experiences persistent pain, your nervous system remains in a heightened state of alert, continuously releasing stress hormones like cortisol and adrenaline. This prolonged activation of the stress response system can lead to anxiety, depression, and other mood disorders.
Research from the National Institute of Health demonstrates that chronic pain patients are three to four times more likely to develop depression. The relationship works bidirectionally—pain causes psychological distress, and psychological distress can intensify pain perception through a phenomenon called central sensitization. This creates a challenging cycle where untreated pain perpetuates mental health struggles, and untreated mental health issues exacerbate pain symptoms.
Sleep disruption represents another critical pathway connecting physical pain to mental health deterioration. Chronic spinal pain often prevents restful sleep, which is essential for emotional regulation, cognitive function, and immune system health. Poor sleep quality amplifies pain perception while simultaneously increasing vulnerability to depression and anxiety. By addressing the underlying physical cause through spinal decompression, patients often experience improvements in sleep quality, creating positive cascading effects on mental well-being.
How Spinal Decompression Reduces Physical Pain
The mechanism by which spinal decompression alleviates pain involves several interconnected physiological processes. When intervertebral discs herniate or become compressed, they press on nerve roots, causing radiating pain, numbness, and weakness. Spinal decompression therapy works by creating negative pressure that gently retracts disc material away from compressed nerves.
This process occurs through a carefully calibrated stretching protocol. The specialized equipment applies tension gradually, allowing the spine to decompress without triggering protective muscle contractions. As the pressure decreases, several beneficial changes occur: increased blood flow to damaged tissues, enhanced nutrient delivery to discs, improved lymphatic drainage of inflammatory substances, and reduced nerve irritation.
Studies published in peer-reviewed journals show that spinal decompression can reduce herniated disc material by up to 6-7 millimeters, representing significant mechanical relief for compressed nerves. Patients typically report pain reduction within 2-4 weeks of beginning treatment, though optimal results usually emerge after completing a full course of therapy. The gradual nature of improvement often translates into sustained relief rather than temporary symptom masking, as seen with pain medications.
When combined with appropriate therapy goals and exercise protocols, spinal decompression creates an environment conducive to tissue healing. This multifaceted approach addresses not just symptom management but actual structural restoration, providing patients with hope and confidence in their recovery trajectory.
Mental Health Benefits Beyond Pain Relief
The mental health improvements associated with successful spinal decompression therapy extend far beyond simple pain relief. When chronic pain subsides, patients experience a profound psychological shift. The constant mental burden of managing pain—anticipating flare-ups, limiting activities, and maintaining focus despite discomfort—finally lifts. This cognitive relief alone significantly improves mood, concentration, and overall quality of life.
Patients undergoing successful spinal decompression frequently report increased energy levels, improved motivation, and renewed engagement with activities they had abandoned due to pain. This restoration of function directly impacts self-esteem and sense of agency. Rather than feeling defined by their condition, patients begin reclaiming their identity as active, capable individuals. This psychological transformation often proves as significant as the physical recovery.
The reduction in anxiety represents another crucial mental health benefit. Chronic pain patients often develop anticipatory anxiety, constantly worrying about pain flare-ups and activity limitations. As spinal decompression reduces pain and improves predictability of function, this anxiety naturally diminishes. Patients regain confidence in their bodies and feel empowered to engage in social activities, exercise, and work without fear of exacerbating their condition.
Additionally, successful pain management through non-pharmacological means like spinal decompression eliminates concerns about medication dependency. Many chronic pain patients struggle with anxiety about opioid use, potential addiction, and long-term medication side effects. Choosing a non-invasive, non-pharmaceutical intervention provides psychological reassurance and aligns with patients’ preferences for natural healing approaches.
Exploring complementary wellness options, such as specialized therapy services and red light therapy near me, can further enhance the mental health benefits achieved through spinal decompression by addressing multiple dimensions of well-being simultaneously.
Research Evidence and Clinical Studies
Scientific evidence supporting spinal decompression’s effectiveness continues accumulating. A landmark study published in the Journal of Back and Musculoskeletal Rehabilitation found that 71% of patients experienced significant pain reduction with spinal decompression therapy. Importantly, many of these patients maintained improvement at long-term follow-up, suggesting lasting benefits rather than temporary relief.
Research examining the psychological components of spinal decompression outcomes reveals that patients experiencing successful pain reduction demonstrate measurable improvements in depression and anxiety scores. A study tracking patients’ mental health alongside physical outcomes found that psychological well-being improvements correlated strongly with pain reduction magnitude, supporting the direct connection between physical relief and mental health enhancement.
The mechanism of action has been further elucidated through imaging studies. MRI analysis of patients before and after spinal decompression shows measurable disc retraction and reduced nerve compression. These objective physical changes validate patients’ subjective reports of improvement, reinforcing the neurobiological basis for both pain relief and associated mental health benefits.
However, researchers emphasize that outcomes vary based on multiple factors including diagnosis accuracy, treatment protocol adherence, concurrent rehabilitation exercises, and individual physiological variation. This variability underscores the importance of seeking treatment from qualified providers who can assess your specific condition and customize protocols accordingly. When researching spinal decompression therapy near me, prioritize facilities with trained specialists and evidence-based treatment approaches.

Finding Quality Spinal Decompression Therapy Near Me
Locating effective spinal decompression therapy requires careful consideration of provider qualifications, facility equipment, and treatment philosophy. Begin by seeking referrals from your primary care physician, spine specialist, or chiropractor. These professionals can recommend reputable facilities with proven track records of successful outcomes.
When evaluating potential providers, verify that they employ FDA-cleared decompression equipment and that practitioners hold appropriate licensure and certifications. Look for facilities offering comprehensive evaluations that include imaging review, detailed history taking, and thorough physical examination before beginning treatment. Providers should clearly explain the treatment protocol, expected timeline, and realistic outcome projections.
The best spinal decompression therapy integrates multiple treatment modalities. Facilities combining decompression with physical therapy, ergonomic counseling, and lifestyle modification typically achieve superior outcomes. Ask about complementary services available at the facility, as comprehensive care addresses multiple factors contributing to your condition.
Reading patient reviews and requesting to speak with former patients provides valuable insight into real-world outcomes. Pay attention to comments about provider communication, facility cleanliness, equipment quality, and whether patients felt their concerns were genuinely addressed. Trustworthy providers welcome questions and encourage patient participation in the treatment planning process.
Consider visiting the MindLift Daily Blog for additional resources on finding qualified healthcare providers and understanding treatment options. Additionally, explore information about occupational therapy careers to understand the broader landscape of qualified healthcare professionals who may collaborate on your care team.
Complementary Therapies for Holistic Wellness
While spinal decompression addresses the mechanical aspects of spinal pain, complementary therapies enhance overall wellness and mental health outcomes. Physical rehabilitation exercises performed during and after decompression therapy strengthen supporting muscles, improve flexibility, and prevent future episodes. These exercises also provide psychological benefits through increased physical capability and reduced injury anxiety.
Mental health support, whether through counseling or cognitive-behavioral therapy, helps patients process the psychological impact of chronic pain and develop healthy coping mechanisms. Many pain management specialists recommend concurrent mental health support to optimize overall recovery. This integrated approach acknowledges that true healing encompasses both body and mind.
Lifestyle modifications including ergonomic adjustments, stress management techniques, and activity pacing work synergistically with spinal decompression to produce lasting results. Patients who combine decompression therapy with consistent exercise, proper posture, and stress reduction practices demonstrate superior long-term outcomes compared to those relying solely on treatment sessions.
Nutritional support also plays an underappreciated role in spinal health and mental well-being. Anti-inflammatory foods, adequate hydration, and appropriate supplementation support tissue healing while simultaneously improving mood and cognitive function. Some providers incorporate nutritional counseling into comprehensive pain management programs.
Potential Limitations and Considerations
Despite promising outcomes, spinal decompression therapy isn’t universally effective for all patients or conditions. Certain diagnoses—such as severe osteoarthritis with bone-on-bone contact, spinal instability, or advanced stenosis—may not respond adequately to decompression alone. Accurate diagnosis through proper imaging and clinical evaluation is essential for determining whether spinal decompression represents an appropriate treatment option for your specific condition.
Individual factors including age, overall health status, concurrent medical conditions, and lifestyle habits influence treatment outcomes. Patients with unrealistic expectations may experience disappointment if improvements occur gradually rather than dramatically. Honest communication about realistic timelines and expected outcomes helps establish appropriate expectations and maintain motivation throughout the treatment course.
Cost considerations matter for many patients, as spinal decompression therapy may not be covered by all insurance plans. Verify coverage before beginning treatment and discuss payment options with your provider. Some facilities offer financing plans or sliding scale fees to make treatment more accessible.
The mental health benefits of spinal decompression depend significantly on achieving adequate pain reduction. Patients experiencing minimal physical improvement may not experience corresponding mental health gains, highlighting the importance of selecting qualified providers and following treatment protocols diligently. If progress stalls, discuss alternative approaches with your healthcare team rather than abandoning treatment prematurely.
FAQ
How long does spinal decompression therapy take to show results?
Most patients begin noticing pain reduction within 2-4 weeks of beginning regular treatment sessions. However, optimal results typically emerge after completing a full course of 15-30 sessions. Individual response varies based on condition severity, diagnosis accuracy, and treatment adherence. Some patients experience faster improvement while others require longer treatment periods to achieve significant relief.
Is spinal decompression therapy painful?
Spinal decompression therapy should not be painful. The procedure involves gentle, controlled stretching that most patients find comfortable or even relaxing. If you experience pain during treatment, immediately inform your provider, as this may indicate improper equipment adjustment or an unsuitable diagnosis. Proper treatment protocols prioritize patient comfort throughout the session.
Can spinal decompression therapy cure my condition permanently?
Spinal decompression therapy can provide significant, lasting relief for many patients, but whether it constitutes a permanent cure depends on your specific condition and post-treatment habits. Maintaining proper ergonomics, continuing exercise protocols, and managing stress help prevent recurrence. Some patients experience complete resolution of symptoms while others achieve substantial improvement that enhances quality of life considerably.
What conditions does spinal decompression therapy treat?
Spinal decompression therapy effectively addresses herniated discs, degenerative disc disease, radiculopathy, sciatica, and certain types of stenosis. However, it may not be appropriate for spinal instability, severe arthritis, or other specific conditions. Thorough diagnostic evaluation determines whether your condition qualifies for this treatment approach.
How does spinal decompression therapy improve mental health?
Pain relief directly improves mental health by reducing stress hormone production, improving sleep quality, restoring physical capability, and reducing anxiety. As physical limitations decrease, patients regain confidence and engagement in meaningful activities, producing profound psychological benefits alongside physical recovery. The non-pharmaceutical approach also eliminates medication-related anxiety.
Should I continue physical therapy after completing spinal decompression?
Yes, continuing appropriate physical therapy and exercise after completing decompression treatment significantly improves long-term outcomes. These exercises strengthen supporting muscles, maintain improved flexibility, and help prevent recurrence. Your provider should recommend specific exercises tailored to your condition and functional goals for ongoing maintenance and continued improvement.


