
Is Mindfulness Useful in Physical Therapy? Expert View
The integration of mindfulness into physical therapy represents one of the most significant developments in rehabilitation medicine over the past decade. As a physical therapy major or practicing clinician, you’ve likely encountered questions about whether mindfulness techniques genuinely enhance patient outcomes or represent merely a trendy addition to treatment protocols. The evidence suggests that mindfulness is far more than a wellness buzzword—it’s a scientifically-supported approach that can meaningfully improve pain perception, movement quality, and long-term adherence to rehabilitation programs.
Modern physical therapy has evolved beyond pure mechanical intervention. Today’s best practitioners recognize that the mind-body connection profoundly influences healing trajectories. Mindfulness-based approaches address this holistic reality by helping patients develop awareness of their bodies, reduce pain-related anxiety, and cultivate the mental resilience necessary for successful recovery. Whether you’re exploring physical therapy career opportunities or refining your clinical skills, understanding mindfulness’s role in rehabilitation is essential.
What Is Mindfulness in Physical Therapy Context
Mindfulness, defined as non-judgmental present-moment awareness, has become increasingly recognized as a legitimate therapeutic tool within rehabilitation settings. In physical therapy specifically, mindfulness refers to intentional attention to bodily sensations, movement patterns, and emotional responses during treatment and home exercise programs. This differs fundamentally from traditional approaches that focus solely on biomechanical correction or strength development.
The application involves teaching patients to observe their bodies without judgment, notice subtle changes in sensation and function, and develop curiosity about their pain rather than fear or avoidance. A patient performing exercises with mindful awareness, for example, might notice how tension patterns shift or how breathing influences movement quality. This heightened somatic awareness becomes a powerful diagnostic and therapeutic tool.
Clinical mindfulness in physical therapy includes several specific techniques: body scans during rehabilitation sessions, mindful breathing integrated into movement patterns, attention-based pain observation, and acceptance-based approaches to discomfort. These practices complement traditional interventions like manual therapy, strengthening exercises, and functional training. The synergy between mechanical intervention and mindful awareness creates a more comprehensive treatment package.

Scientific Evidence Supporting Mindfulness Integration
Research from leading institutions demonstrates compelling support for mindfulness-based interventions in physical rehabilitation. A landmark study published in JAMA Internal Medicine found that mindfulness-based stress reduction programs produced outcomes comparable to pharmaceutical interventions for chronic pain conditions. This finding carries significant implications for physical therapy, where chronic pain frequently complicates recovery.
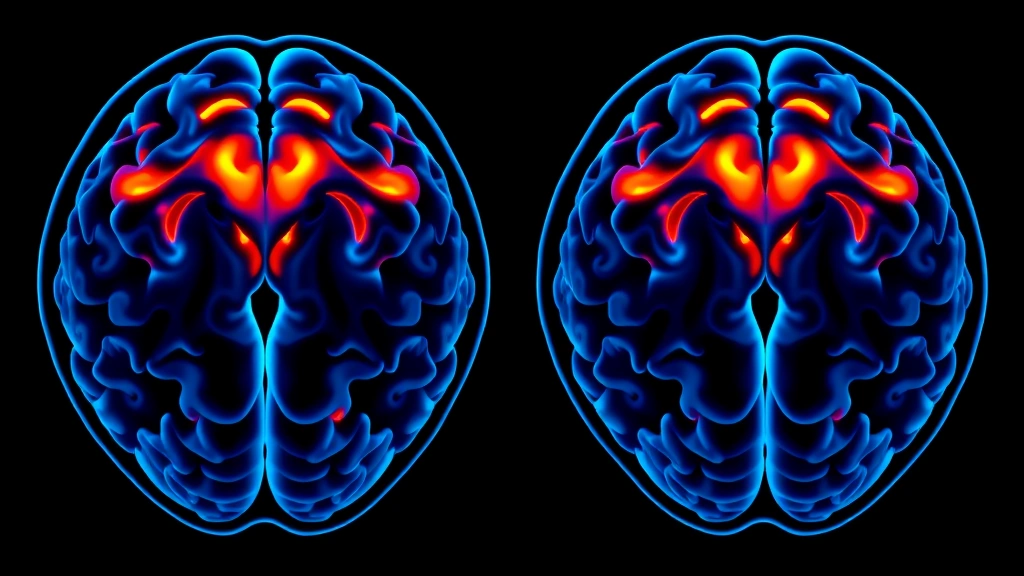
The National Center for Biotechnology Information hosts extensive research demonstrating that mindfulness practice produces measurable neurological changes. Brain imaging studies show that regular mindfulness meditation alters activity in regions associated with pain processing, emotional regulation, and self-awareness. These aren’t merely subjective improvements—they reflect genuine neurobiological adaptation.
A systematic review in Pain Medicine Journal examined 38 randomized controlled trials involving mindfulness-based interventions for pain management. The analysis concluded that mindfulness techniques consistently reduced pain intensity ratings by 15-30% across diverse patient populations. Furthermore, improvements persisted at six-month and twelve-month follow-ups, suggesting lasting neurological changes rather than temporary placebo effects.
Research from the American Psychological Association indicates that mindfulness improves emotional regulation, which directly impacts pain perception. Patients who develop mindfulness skills show reduced catastrophizing—the tendency to assume the worst about pain—and decreased fear-avoidance behaviors that typically prolong disability.
Pain Management and Perception Reduction
One of mindfulness’s most valuable contributions to physical therapy involves fundamentally changing how patients relate to pain. Traditional pain management often emphasizes elimination or avoidance; mindfulness-based approaches teach patients that pain perception can be modified through attention and attitude, even when tissue damage remains constant.
The neuroscience underlying this phenomenon is well-established. Pain is not simply a direct response to tissue damage but rather a complex construction involving sensory input, attention, emotion, memory, and belief. By teaching patients to observe pain sensations with curiosity rather than fear, mindfulness reduces the suffering component of pain while potentially reducing intensity itself.
Consider a patient recovering from an ACL reconstruction experiencing post-surgical pain. A traditional approach might rely on pain medication and rest. A mindfulness-integrated approach teaches the patient to distinguish between the sensation itself and the story they’re telling about it. Rather than “this pain means something is wrong,” the patient learns “this is a sensation; it’s uncomfortable, and it’s also part of the healing process.” This cognitive shift produces measurable reductions in perceived pain severity.
Research demonstrates that mindfulness reduces pain catastrophizing by 40-50% in rehabilitation populations. When patients stop anticipating worse pain or viewing their condition as hopeless, they become more willing to engage in therapeutic exercises, leading to superior functional outcomes. The psychological shift becomes a mechanism for physical improvement.
Mindfulness-based pain management proves particularly valuable for patients with conditions like hip labrum tears, where pain sensitivity and fear-avoidance significantly impact recovery trajectories. Patients who learn to modulate their pain perception through mindfulness typically progress faster through rehabilitation phases and achieve better long-term functional outcomes.
Improving Patient Compliance and Outcomes
Exercise adherence represents one of the greatest challenges in physical therapy. Studies consistently show that 50-70% of patients fail to complete prescribed home exercise programs, undermining treatment effectiveness. Mindfulness addresses this critical compliance problem through multiple mechanisms.
First, mindfulness improves the patient-therapist relationship. When clinicians teach mindfulness skills and demonstrate genuine interest in patients’ subjective experiences, therapeutic alliance strengthens. Patients feel understood and valued, increasing motivation to follow recommendations. This relational component shouldn’t be underestimated—it’s a primary driver of adherence.
Second, mindfulness transforms exercise compliance from an external obligation into an intrinsically motivated practice. Patients who approach exercises mindfully—noticing sensations, observing improvements, and appreciating their body’s capacity—develop genuine interest in continuing. The activity becomes rewarding in itself rather than a burdensome requirement.
Third, mindfulness reduces the anxiety and catastrophic thinking that often prevent patients from pushing themselves appropriately during rehabilitation. Many patients unconsciously limit their activity due to fear of re-injury, even after tissue healing is complete. Mindfulness teaches them to distinguish between genuine warning signals and anxiety-driven false alarms, allowing appropriate progression.
Research indicates that patients receiving mindfulness-integrated physical therapy show 25-35% better adherence to home programs compared to standard treatment groups. This superior compliance translates directly to improved outcomes: faster functional recovery, reduced re-injury rates, and greater long-term satisfaction with treatment.
Practical Implementation Strategies for Clinicians
Implementing mindfulness in physical therapy doesn’t require extensive retraining or major practice restructuring. Clinicians can begin with simple, evidence-based techniques that integrate naturally into existing treatment protocols.
Body Scan Integration: Begin treatment sessions with two-minute body scans where patients systematically notice sensations throughout their body. This establishes baseline awareness and helps identify compensatory tension patterns. Patients learn to recognize their habitual holding patterns, which then become targets for release during treatment.
Mindful Movement: Have patients perform therapeutic exercises with deliberate attention to sensation and movement quality rather than rushing through repetitions. Slow movements with focused awareness produce superior motor learning compared to rapid, mindless repetitions. This approach proves particularly valuable for physical therapy education students learning to teach proper technique.
Breathing Awareness: Teach patients to coordinate breathing with movement and to use breath as an anchor for attention. Conscious breathing reduces tension, improves movement efficiency, and provides a portable tool patients can use independently between sessions.
Pain Observation Practice: Rather than asking patients to rate pain on a scale, teach them to observe pain sensations with curiosity. Where exactly is it located? What’s the texture? Does it change with movement or breathing? This observational stance reduces emotional reactivity while providing valuable clinical information.
Progressive Relaxation: Teach patients to systematically tense and release muscle groups, developing awareness of the contrast between tension and relaxation. This technique improves proprioceptive awareness while directly reducing muscular tension.
These techniques require minimal additional time but dramatically enhance treatment effectiveness. A five-minute mindfulness component integrated into a standard 50-minute session can significantly improve outcomes without increasing appointment length.
Mindfulness for Specific Conditions
While mindfulness benefits diverse patient populations, certain conditions show particularly dramatic responses to mindfulness-integrated treatment.
Chronic Pain Syndromes: Patients with fibromyalgia, chronic fatigue, and widespread pain respond exceptionally well to mindfulness approaches. These conditions involve central sensitization—amplified pain signaling—that mindfulness directly addresses through attention retraining and emotional regulation.
Post-Surgical Rehabilitation: Mindfulness reduces post-operative pain perception and anxiety while improving surgical outcomes. Patients who practice mindfulness before surgery show reduced opioid requirements and faster functional recovery afterward.
Neurological Conditions: Stroke patients, those with Parkinson’s disease, and individuals recovering from traumatic brain injury benefit from mindfulness-enhanced rehabilitation. The attention-training aspects of mindfulness support neurological recovery and neuroplasticity.
Movement Disorders: Patients with tension headaches, dystonia, and movement-related pain conditions often suffer from excessive muscle tension driven by psychological factors. Mindfulness directly addresses these psychosomatic components.
Occupational Injuries: Workers with repetitive strain injuries benefit from mindfulness training that helps them recognize and release habitual tension patterns. This prevents recurrence after treatment completion.
While exploring various therapy career paths, such as occupational therapy positions or speech therapy opportunities, understanding how mindfulness applies across disciplines becomes increasingly valuable. Similarly, exploring complementary approaches like music therapy education reveals how mindfulness principles integrate across therapeutic modalities.
Training and Certification Considerations
Physical therapists interested in developing expertise in mindfulness-based approaches have several evidence-based training options. The Center for Mindfulness at University of Massachusetts Medical School offers Mindfulness-Based Stress Reduction (MBSR) certification programs specifically designed for healthcare professionals. These programs provide both personal practice experience and clinical training.
The International Association of Yoga Therapists and various physical therapy associations offer specialized training in yoga-informed physical therapy and mindfulness integration. These programs typically require 100-200 hours of training beyond basic PT credentials but provide comprehensive competency in clinical application.
For physical therapy professionals seeking to integrate mindfulness into their practice, starting with personal meditation practice is essential. Clinicians cannot authentically teach mindfulness without genuine personal experience. Most experts recommend establishing a consistent personal practice before attempting clinical application.
Continuing education units are available through most state physical therapy boards for mindfulness and somatic awareness courses. This ensures that mindfulness training counts toward licensure maintenance requirements, making professional development financially sustainable.
Integrating mindfulness into your physical therapy practice represents both a clinical advancement and a professional differentiator. Patients increasingly seek practitioners who offer comprehensive, evidence-based approaches addressing mind and body. Developing mindfulness expertise positions clinicians as leaders in modern rehabilitation medicine.
FAQ
Is mindfulness suitable for all physical therapy patients?
While mindfulness benefits most patients, certain populations require modified approaches. Patients with acute psychiatric conditions, severe trauma histories, or active psychosis may need specialized guidance or preliminary psychological support before mindfulness practice. For most patients with musculoskeletal conditions, pain syndromes, or post-surgical rehabilitation, mindfulness proves beneficial and safe when properly introduced.
How much mindfulness training do physical therapists need?
Basic mindfulness integration—teaching body awareness and mindful movement—requires minimal additional training beyond reading current literature and practicing personally. However, clinicians working with complex pain syndromes or trauma-affected patients benefit from formal certification programs (typically 100-200 hours). The depth of training should match the complexity of patient populations served.
Does mindfulness replace traditional physical therapy interventions?
No. Mindfulness enhances but doesn’t replace evidence-based physical therapy techniques like manual therapy, therapeutic exercise, and functional training. The most effective approach combines mechanical intervention with mindfulness-based approaches, creating synergistic benefits that exceed either approach alone.
What’s the evidence timeline for mindfulness benefits?
Some benefits appear within single sessions—patients often report reduced pain perception and improved movement quality immediately after mindfulness-integrated treatment. Sustained benefits typically develop over 4-8 weeks of consistent practice. Neurological changes visible on brain imaging require 8-12 weeks of regular mindfulness practice.
Can patients practice mindfulness independently, or do they need professional guidance?
Patients can certainly practice mindfulness independently using apps, books, or online resources. However, professional guidance from trained clinicians ensures proper technique and helps patients navigate challenges. The combination of independent practice and professional guidance produces optimal results.
How does mindfulness affect pain medication requirements?
Research indicates that patients practicing mindfulness often require reduced pain medication doses, particularly for chronic pain conditions. However, medication adjustments should only occur under physician supervision. Mindfulness should complement rather than replace appropriate pharmacological management.



