Is Hyperbaric Oxygen Therapy Effective? Expert Insights and Evidence
Hyperbaric oxygen therapy (HBOT) has gained significant attention in recent years as a potential treatment for various medical conditions. Whether you’re exploring options in St. Johns County or considering this therapy for a specific health concern, understanding its effectiveness is crucial. This comprehensive guide examines the scientific evidence, expert opinions, and practical applications of hyperbaric oxygen therapy to help you make an informed decision about whether it’s the right choice for your situation.
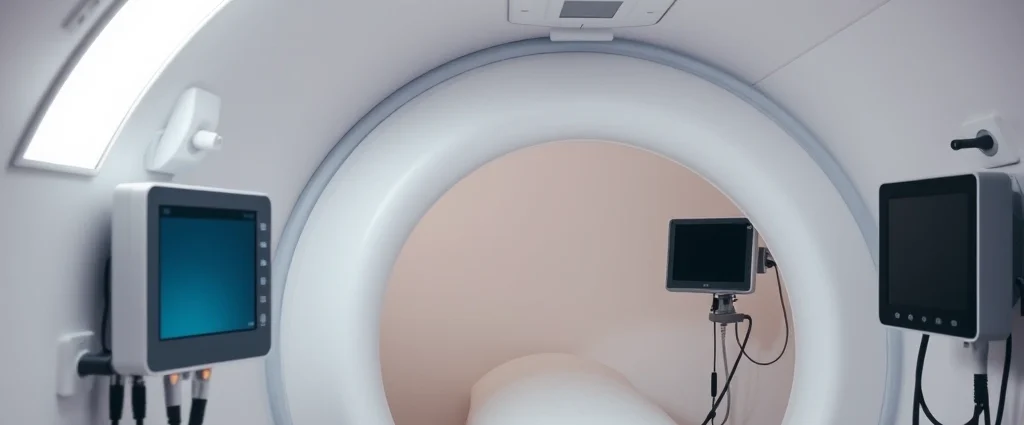
The therapy works by placing patients in a pressurized chamber where they breathe pure oxygen at levels higher than atmospheric pressure. This process increases oxygen saturation in the bloodstream, theoretically promoting healing and reducing inflammation. However, the question remains: does the science support these claims? We’ll explore what research tells us about this treatment modality and its real-world applications.

How Hyperbaric Oxygen Therapy Works
Hyperbaric oxygen therapy operates on a straightforward physiological principle: increased atmospheric pressure combined with high oxygen concentration enhances oxygen diffusion into tissues. During a typical session, patients enter a pressurized chamber—either monoplace (single-occupant) or multiplace (multiple-occupant)—where the air pressure is gradually increased to 2.0 to 3.0 atmospheres absolute (ATA).
At these elevated pressures, oxygen dissolves more effectively into the plasma portion of blood, allowing it to reach areas with compromised circulation or reduced oxygen availability. This process, governed by Henry’s Law, enables oxygen to penetrate tissues that normal atmospheric breathing cannot adequately supply. The therapy typically involves sessions lasting 90 to 120 minutes, with treatment courses ranging from 20 to 40 sessions depending on the condition being treated.
The mechanism extends beyond simple oxygen delivery. Research indicates that HBOT stimulates neovascularization—the formation of new blood vessels—and enhances the body’s natural healing processes. It also reduces inflammation, promotes collagen deposition, and improves white blood cell function, all contributing to tissue repair and regeneration.

Scientific Evidence and Clinical Research
The effectiveness of hyperbaric oxygen therapy varies significantly depending on the condition being treated. According to the FDA, only certain conditions have substantial clinical evidence supporting HBOT as a legitimate treatment. However, numerous studies continue to investigate its potential for various other applications.
A landmark study published in the Cochrane Database of Systematic Reviews examined HBOT for diabetic foot ulcers, finding that the therapy significantly increased healing rates when combined with standard wound care. The research demonstrated approximately 61% complete healing with HBOT compared to 49% without the therapy. For acute crush injuries and carbon monoxide poisoning, evidence is particularly robust, with multiple randomized controlled trials confirming HBOT’s effectiveness in improving outcomes.
The National Institutes of Health and various academic medical centers have conducted extensive research on HBOT mechanisms. These studies reveal that the therapy activates specific genes related to angiogenesis and wound healing, providing molecular-level support for its clinical benefits. However, researchers emphasize that HBOT works best as a complementary therapy rather than a standalone treatment for most conditions.
It’s important to note that while some studies show promising results for conditions like fibromyalgia, autism spectrum disorder, and traumatic brain injury, the evidence for these applications remains preliminary. The scientific community continues to call for larger, well-designed clinical trials to establish definitive efficacy for off-label uses.
FDA-Approved Conditions
The FDA has formally approved hyperbaric oxygen therapy for a specific list of conditions where clinical evidence strongly supports its use. These include:
- Diabetic foot ulcers (Wagner Grade 3 or higher)
- Chronic osteomyelitis and other refractory bone infections
- Acute traumatic ischemia from crush injuries
- Decompression sickness (the bends)
- Carbon monoxide poisoning
- Severe anemia when blood transfusion isn’t possible
- Arterial insufficiencies and compromised grafts
- Gangrene and necrotizing soft tissue infections
- Radiation tissue damage (osteoradionecrosis)
- Thermal burns (third-degree)
- Exceptional blood loss anemia
For these conditions, insurance typically covers HBOT treatments as a medically necessary intervention. When seeking hyperbaric oxygen therapy in Palm Coast or other locations, patients with FDA-approved diagnoses have better prospects for coverage and reimbursement.
Off-Label Uses and Emerging Applications
Beyond FDA-approved indications, researchers and clinicians have explored HBOT for numerous other conditions. While the evidence for these applications is developing, some show encouraging preliminary results. These off-label uses include:
Neurological conditions: Some studies suggest HBOT may improve outcomes in traumatic brain injury and spinal cord injury by reducing inflammation and promoting neuroplasticity. Autism spectrum disorder research has generated mixed results, with some studies showing behavioral improvements while others found minimal effects.
Chronic wounds: Beyond diabetic foot ulcers, HBOT shows promise for various chronic wounds, including pressure ulcers and venous leg ulcers, particularly when combined with standard wound care protocols.
Sports medicine and recovery: Athletes have increasingly sought HBOT for injury recovery, though the scientific evidence for performance enhancement remains limited. Some professional sports organizations have invested in HBOT facilities despite inconclusive research.
Post-operative healing: Emerging research suggests HBOT may accelerate healing following cosmetic and reconstructive surgery, though well-designed trials are still needed.
Radiation side effects: HBOT shows promise in managing radiation-induced tissue damage, a recognized FDA-approved use that extends to various cancer treatment complications.
When considering HBOT for conditions outside FDA approval, patients should understand that insurance coverage is unlikely and outcomes are not guaranteed. Consulting with qualified healthcare providers becomes especially important in these scenarios.
Hyperbaric Oxygen Therapy in St. Johns County
St. Johns County residents have access to several facilities offering hyperbaric oxygen therapy. When searching for providers in this area, it’s essential to verify that facilities meet rigorous safety standards and employ certified hyperbaric medicine specialists.
Quality HBOT centers should have:
- Board-certified hyperbaric medicine physicians overseeing treatment
- Properly maintained and regularly inspected chambers
- Comprehensive patient screening and evaluation protocols
- Trained hyperbaric technicians and nursing staff
- Clear protocols for emergency situations
- Detailed documentation and progress tracking
Local providers can offer personalized treatment plans tailored to your specific condition and health status. If you’re exploring HBOT options in St. Johns County, ask potential providers about their experience with your particular diagnosis and request references from other patients.
For those seeking additional information about local options, resources like the MindLift Daily Blog featuring therapy resources and information can help guide your research. Additionally, understanding how long the effects of hyperbaric oxygen therapy last helps with treatment planning and expectations management.
Safety Considerations and Potential Side Effects
While hyperbaric oxygen therapy is generally considered safe when administered by qualified professionals, certain risks warrant attention. Most side effects are mild and temporary, including:
- Barotrauma: Pressure-related ear or sinus discomfort, typically managed through equalization techniques
- Oxygen toxicity: Rare but serious; occurs when oxygen levels become excessive, potentially causing seizures
- Claustrophobia: Anxiety related to the enclosed chamber environment
- Myopia: Temporary nearsightedness that usually resolves after treatment completion
- Fatigue: Mild tiredness following sessions
- Dehydration: Increased fluid loss during pressurization
Certain medical conditions contraindicate HBOT or require careful monitoring. These include uncontrolled fever, upper respiratory infections, and specific medications like cisplatin. Patients with claustrophobia may find multiplace chambers more tolerable than monoplace units.
Proper pre-treatment screening, including medical history review and physical examination, helps identify potential complications before they occur. Reputable facilities conduct thorough assessments and provide detailed informed consent documentation.
Comparing HBOT to Other Therapies
When evaluating treatment options, understanding how HBOT compares to alternative therapies proves valuable. For diabetic foot ulcers, HBOT combined with standard wound care outperforms wound care alone, but comparable results may be achieved through aggressive infection management, debridement, and specialized dressings in some cases.
Similar to how red light therapy for back pain offers a non-invasive alternative for certain conditions, HBOT provides a non-pharmacological approach to healing. However, HBOT requires more time commitment and has higher upfront costs than many alternatives.
For acute conditions like carbon monoxide poisoning or decompression sickness, HBOT stands as the gold standard with no practical alternatives. For chronic conditions, treatment decisions should consider efficacy, cost, time commitment, and individual patient factors.
Physical rehabilitation approaches, such as physical therapy for shoulder pain, often complement HBOT rather than replace it. Integrating multiple therapeutic modalities frequently produces superior outcomes compared to single-intervention approaches.
The choice between HBOT and alternatives should involve discussions with qualified healthcare providers who understand your specific condition, medical history, and treatment goals. Evidence-based decision-making, combined with personalized medical guidance, leads to optimal outcomes.
Frequently Asked Questions
What conditions does hyperbaric oxygen therapy treat most effectively?
HBOT demonstrates the strongest evidence for diabetic foot ulcers, carbon monoxide poisoning, decompression sickness, and acute traumatic ischemia. For FDA-approved conditions, effectiveness rates typically range from 60-85% depending on the specific diagnosis and individual factors. Off-label applications show more variable results and should be approached cautiously.
How many sessions are typically required?
Treatment courses vary by condition. Most patients receive 20 to 40 sessions, with some conditions requiring fewer sessions and others potentially requiring more. Sessions typically last 90-120 minutes, conducted 5 days per week. Your healthcare provider will recommend a specific protocol based on your diagnosis and response to treatment.
Is hyperbaric oxygen therapy covered by insurance?
Insurance coverage depends on whether your condition is FDA-approved and whether your specific insurance plan covers HBOT. Most major insurance providers cover treatment for FDA-approved conditions when prescribed by qualified physicians. Off-label uses are rarely covered. Always verify coverage with your insurance provider before beginning treatment.
Can hyperbaric oxygen therapy cure my condition?
HBOT functions best as a therapeutic tool that supports healing rather than a cure. For acute conditions like carbon monoxide poisoning, it can completely resolve the problem. For chronic conditions, HBOT typically improves healing rates and outcomes but works optimally as part of comprehensive treatment plans including standard medical care.
Are there any long-term side effects from hyperbaric oxygen therapy?
Long-term complications are rare with proper administration. The most common persistent effect is temporary myopia (nearsightedness) that usually resolves after treatment completion. Serious long-term effects are exceptionally uncommon when treatment is provided by qualified professionals in certified facilities.
How does hyperbaric oxygen therapy compare to other emerging therapies?
HBOT has decades of research supporting specific applications, whereas many emerging therapies lack extensive clinical evidence. This established track record provides greater confidence in outcomes for FDA-approved uses. For other conditions, newer therapies may show promise but typically have less comprehensive evidence than HBOT.
Can I combine hyperbaric oxygen therapy with other treatments?
Yes, HBOT works well as a complementary therapy alongside standard medical treatments. In fact, many FDA-approved applications involve combining HBOT with conventional care. Always inform all your healthcare providers about HBOT to ensure treatments complement rather than interfere with each other.