Is Hyperbaric Oxygen Therapy Effective? Expert Insights and Evidence-Based Analysis
Hyperbaric oxygen therapy (HBOT) has gained significant attention in recent years as a potential treatment for various medical conditions, from wound healing to neurological disorders. However, separating fact from marketing hype requires a careful examination of the scientific evidence. This comprehensive guide explores what hyperbaric oxygen therapy is, how it works, which conditions it effectively treats, and what the research actually tells us about its efficacy.
If you’re considering hyperbaric oxygen therapy in Mount Vernon, WA, or anywhere else, understanding the evidence behind this treatment is essential. We’ll examine clinical studies, expert opinions, and real-world applications to help you make informed decisions about whether HBOT might be appropriate for your specific health concerns.
What Is Hyperbaric Oxygen Therapy?
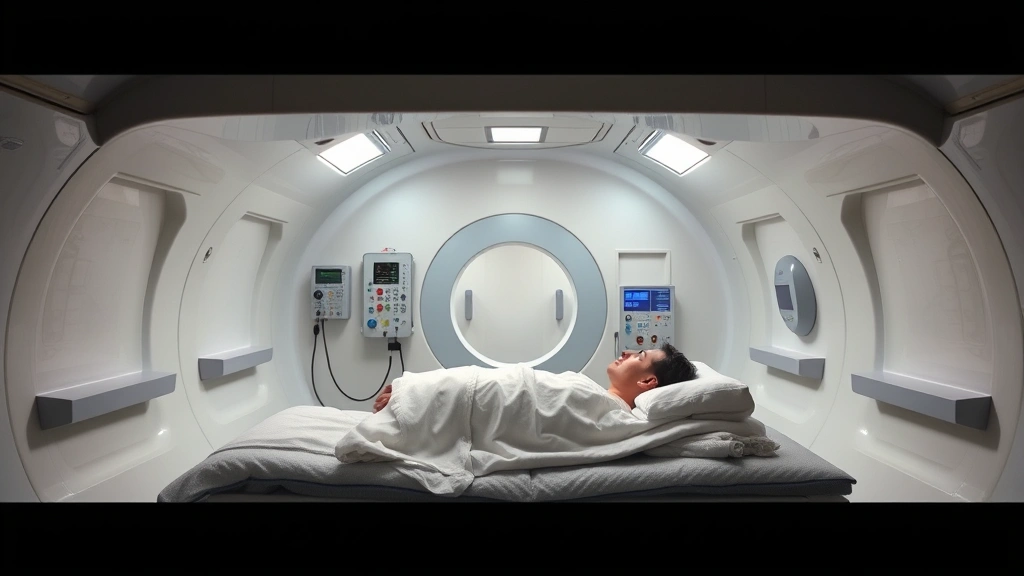
Hyperbaric oxygen therapy is a medical treatment in which patients breathe pure oxygen in a pressurized chamber. The pressure inside the chamber is typically two to three times greater than normal atmospheric pressure at sea level. This increased pressure allows the lungs to gather more oxygen than would be possible when breathing pure oxygen at normal air pressure.
The therapy was first used in the 1600s but gained medical legitimacy in the twentieth century when researchers discovered its effectiveness for treating decompression sickness in divers. Today, hyperbaric oxygen therapy in Mount Vernon, WA and other locations uses either monoplace chambers (single-occupant) or multiplace chambers (multiple occupants), with sessions typically lasting between 90 minutes and 2 hours.
The basic principle is straightforward: increased oxygen partial pressure in the blood promotes healing by enhancing the body’s natural repair mechanisms. However, the specific conditions that benefit from this mechanism have been the subject of extensive medical research and debate.
How Does HBOT Work Scientifically?
Understanding the mechanism of action is crucial to evaluating hyperbaric oxygen therapy’s effectiveness. When you breathe pure oxygen under pressure, the amount of oxygen dissolved in your blood plasma increases dramatically. This is distinct from oxygen bound to hemoglobin; the dissolved oxygen reaches areas of tissue that may have compromised circulation.
At the cellular level, increased oxygen availability supports several important processes. First, it enhances physical therapy outcomes by improving tissue oxygenation during recovery. Second, elevated oxygen levels stimulate angiogenesis—the formation of new blood vessels—which is particularly valuable in tissues with poor circulation. Third, HBOT reduces inflammation and modulates immune function, potentially accelerating healing responses.
Research published in the Journal of Wound Care and other peer-reviewed journals demonstrates that HBOT increases oxygen tensions in hypoxic tissues, creating an environment conducive to collagen deposition, fibroblast proliferation, and epithelialization. However, these cellular benefits don’t automatically translate to clinical effectiveness for every condition. The presence of a biological mechanism doesn’t guarantee therapeutic benefit in human populations.
A critical consideration is that these effects are most pronounced in tissues with compromised oxygen delivery. In healthy tissues with normal circulation, additional oxygen provides minimal benefit. This distinction explains why HBOT shows effectiveness for certain conditions while failing to demonstrate benefit for others.
FDA-Approved Conditions and Evidence
The U.S. Food and Drug Administration has approved hyperbaric oxygen therapy for a specific list of conditions based on substantial clinical evidence. These approved indications represent treatments where HBOT has demonstrated clear efficacy in rigorous clinical trials.
Approved indications include:
- Decompression sickness (the bends)
- Gas embolism
- Acute traumatic peripheral ischemia
- Chronic wounds, particularly diabetic foot ulcers
- Severe anemia when transfusion is refused or unavailable
- Intracranial abscess
- Necrotizing soft tissue infections
- Osteomyelitis and compromised grafts/flaps
- Radiation tissue damage (osteoradionecrosis)
- Sudden sensorineural hearing loss
For diabetic foot ulcers specifically, multiple randomized controlled trials have demonstrated that HBOT reduces amputation risk and accelerates wound closure when combined with standard wound care. A landmark study in Diabetes Care found that HBOT reduced the risk of major amputation by approximately 50% in patients with Wagner grade 3 or higher foot ulcers.
The evidence for sudden sensorineural hearing loss is more nuanced. While some studies show benefit, particularly when treatment begins within two weeks of symptom onset, whether therapy works for hearing loss remains somewhat controversial in the medical community. A 2018 Cochrane review concluded that evidence was insufficient to confirm HBOT’s effectiveness for this indication, though many audiologists report clinical success.

Off-Label Uses and Clinical Research
Beyond FDA-approved conditions, HBOT is sometimes used off-label for conditions including traumatic brain injury, autism spectrum disorder, cerebral palsy, fibromyalgia, and chronic fatigue syndrome. The evidence for these applications is considerably weaker and remains controversial.
Several studies have examined HBOT for traumatic brain injury and post-concussion syndrome. A 2013 study in Medical Gas Research suggested potential benefits for chronic brain injury patients, but larger, more rigorous trials have produced mixed results. The challenge is that brain injury involves complex neurochemical and structural changes that may not respond uniformly to increased oxygen availability.
For autism spectrum disorder, some clinicians have promoted HBOT based on the theory that autistic individuals have impaired cerebral blood flow. However, research from major autism research organizations has found insufficient evidence to support HBOT as an effective autism treatment. The American Academy of Pediatrics does not recommend HBOT for autism.
Similarly, claims about HBOT treating fibromyalgia and chronic fatigue syndrome lack robust clinical evidence. While small studies have occasionally reported subjective improvements, larger controlled trials have failed to demonstrate significant benefit beyond placebo effects. This highlights an important principle: perceived improvement doesn’t necessarily indicate true therapeutic efficacy.
The distinction between FDA-approved and off-label uses is significant. Approved indications have withstood rigorous scrutiny and demonstrated consistent benefit across multiple well-designed studies. Off-label uses may have preliminary evidence or theoretical justification, but they lack the robust clinical validation that should guide treatment decisions.
Safety Considerations and Side Effects
Hyperbaric oxygen therapy is generally considered safe when administered by trained professionals in properly maintained chambers. However, like all medical treatments, it carries potential risks that patients should understand.
Common side effects include:
- Barotrauma (pressure-related ear and sinus injuries)
- Myopia (temporary nearsightedness)
- Fatigue
- Claustrophobia and anxiety
- Oxygen toxicity (rare but serious)
- Hypoglycemia in diabetic patients
Oxygen toxicity, also called central nervous system oxygen toxicity, is the most serious potential complication. Breathing pure oxygen under high pressure can cause seizures, though this occurs in fewer than 2% of treatments. Proper protocols, including air breaks during long sessions, minimize this risk significantly.
Barotrauma occurs when pressure changes damage the middle ear or sinuses. Most cases are mild and resolve without intervention, but severe barotrauma can cause permanent hearing loss. Patients with Eustachian tube dysfunction face higher risk and should be carefully screened.
Myopia typically develops during HBOT courses due to lens swelling from increased oxygen saturation. This is usually temporary, resolving within weeks to months after treatment concludes. However, some patients experience permanent refractive changes.
Diabetic patients require special monitoring because HBOT can rapidly lower blood glucose levels, potentially causing dangerous hypoglycemic episodes. Careful glucose monitoring and medication adjustment are essential.

HBOT in Mount Vernon, Washington
For residents of Mount Vernon, Washington, accessing hyperbaric oxygen therapy involves identifying qualified medical facilities. When seeking HBOT treatment locally, several factors warrant consideration.
First, verify that the facility is staffed by physicians certified in hyperbaric medicine through recognized organizations like the American Board of Medical Specialties. The treating physician should conduct a thorough evaluation to determine whether your specific condition falls within evidence-based indications for HBOT.
Second, confirm that the facility maintains proper safety protocols and equipment maintenance standards. Reputable centers follow Undersea and Hyperbaric Medical Society (UHMS) guidelines and maintain current certifications.
Third, understand your insurance coverage. Medicare and most private insurers cover HBOT for FDA-approved indications but typically deny coverage for off-label uses. Clarifying coverage before beginning treatment prevents unexpected financial burdens.
If you’re considering HBOT in Mount Vernon, WA, discuss your condition thoroughly with your primary care physician and any relevant specialists. They can help determine whether HBOT is appropriate and coordinate care with hyperbaric specialists. For those interested in exploring this option, resources about hyperbaric oxygen therapy in Mount Vernon, WA provide local facility information.
Comparing HBOT to Other Therapies
When evaluating treatment options, comparing HBOT to alternative therapies provides important context. For many conditions, multiple evidence-based treatments exist, and HBOT may be one component of a comprehensive approach.
For diabetic foot ulcers, for example, the foundation of treatment remains meticulous wound care, infection management, and glycemic control. HBOT enhances these standard approaches but doesn’t replace them. Similarly, red light therapy for back pain and other emerging therapies should be evaluated against established treatments with proven efficacy.
The cost of physical therapy and other established treatments should also factor into decision-making. HBOT typically costs between $1,500 and $3,000 per session or $10,000 to $30,000 for a typical course of 20-40 treatments. Insurance coverage varies significantly based on diagnosis.
For conditions like traumatic brain injury, physical therapy, cognitive rehabilitation, and psychological support have substantially more evidence supporting their effectiveness than HBOT. A comprehensive treatment plan typically combines multiple evidence-based approaches rather than relying on any single therapy.
External research from the Cochrane Library provides systematic reviews of HBOT efficacy for various conditions, offering comprehensive summaries of available evidence. Additionally, the National Center for Biotechnology Information (NCBI) PubMed database contains thousands of peer-reviewed studies examining HBOT outcomes.
The Undersea and Hyperbaric Medical Society (UHMS) maintains current clinical practice guidelines based on systematic review of evidence. Their official indications represent the most authoritative consensus on when HBOT demonstrates proven efficacy.
Research from the Wound Healing Society and published in journals like Advances in Wound Care continues to refine understanding of HBOT’s role in treating chronic wounds. Recent meta-analyses confirm benefit for specific wound types while questioning efficacy for others.
Frequently Asked Questions
How many HBOT sessions are typically needed?
Treatment duration varies based on diagnosis. Acute conditions like decompression sickness may require 5-20 sessions, while chronic wounds typically require 20-40 sessions. Your physician will establish a specific treatment plan based on your condition and response to therapy.
Can HBOT be used alongside other medications?
Generally yes, but certain medications require adjustment. Disulfiram (Antabuse), cisplatin, and doxorubicin may interact with HBOT. Always inform your hyperbaric physician about all medications and supplements you’re taking.
Is HBOT covered by insurance?
Medicare and most private insurers cover HBOT for FDA-approved indications. Coverage for off-label uses is rarely provided. Contact your insurance company and the treatment facility to clarify your coverage before beginning therapy.
How long do HBOT effects last?
For acute conditions, benefits are typically permanent once healing is complete. For chronic conditions, some patients experience gradual improvement that persists long-term, while others may require periodic maintenance sessions. Individual responses vary considerably.
What makes HBOT different from breathing oxygen at home?
The pressure is the crucial difference. Breathing supplemental oxygen at home increases blood oxygen levels modestly, while HBOT dramatically increases dissolved oxygen in blood plasma by 15-20 times. This substantial difference enables therapeutic effects impossible to achieve with home oxygen alone.
Are there any conditions where HBOT is contraindicated?
Untreated claustrophobia, uncontrolled fever, and certain chemotherapy regimens may contraindicate HBOT. Thorough medical evaluation identifies any contraindications before treatment begins. Most patients tolerate HBOT well when properly screened.



