
Is Hyperbaric Oxygen Therapy Effective? Expert Insights
Hyperbaric oxygen therapy (HBOT) has gained significant attention in recent years as a potential treatment for various medical conditions. This specialized medical procedure involves breathing pure oxygen in a pressurized chamber, allowing your lungs to gather more oxygen than would be possible breathing air at normal atmospheric pressure. The therapy has been used for decades, initially to treat decompression sickness in divers, but its applications have expanded considerably. For residents in Mount Vernon, WA, and surrounding areas seeking alternative therapeutic approaches, understanding the evidence behind HBOT is essential for making informed healthcare decisions.
The fundamental principle behind hyperbaric oxygen therapy is straightforward yet powerful: increased oxygen availability promotes healing at the cellular level. When your body is exposed to pressures two to three times greater than normal atmospheric pressure while breathing pure oxygen, your blood plasma becomes saturated with dissolved oxygen. This enhanced oxygen delivery reaches tissues that may be oxygen-deprived due to injury, infection, or chronic disease. However, the question of whether HBOT truly delivers on its promises requires careful examination of clinical evidence, expert opinions, and documented outcomes.
How Hyperbaric Oxygen Therapy Works
Understanding the mechanics of hyperbaric oxygen therapy requires knowledge of basic physiology and pressure dynamics. During a standard HBOT session, you enter a pressurized chamber—either monoplace (single-occupant) or multiplace (multiple-occupant)—where atmospheric pressure gradually increases to 2.4 to 3.0 atmospheres absolute (ATA). At these elevated pressures, your lungs can extract significantly more oxygen from the breathing gas.
The dissolved oxygen in your blood plasma becomes the key mechanism of action. Under normal atmospheric conditions, oxygen travels primarily bound to hemoglobin in red blood cells. However, at hyperbaric pressures, substantial amounts of oxygen dissolve directly into plasma, cerebrospinal fluid, and other body fluids. This dissolved oxygen can reach areas with compromised blood flow, such as scar tissue, radiation-damaged areas, or tissues affected by chronic wounds. The increased oxygen availability stimulates several biological responses: enhanced white blood cell function for fighting infection, promotion of collagen synthesis for wound healing, and stimulation of new blood vessel formation (angiogenesis).
Typical treatment protocols involve sessions lasting 90 to 120 minutes, with patients undergoing multiple sessions—often 20 to 40 treatments—depending on their condition. The pressurization and depressurization occur gradually to minimize discomfort and reduce the risk of barotrauma.
FDA-Approved Medical Uses
The Food and Drug Administration has formally approved hyperbaric oxygen therapy for a specific list of conditions where clinical evidence demonstrates clear benefit. These approved indications represent the gold standard for HBOT efficacy:
- Decompression sickness (the bends) in divers exposed to rapid pressure changes
- Gas embolism where air bubbles enter blood vessels
- Carbon monoxide poisoning where HBOT effectively displaces carbon monoxide from hemoglobin
- Chronic wounds particularly diabetic foot ulcers that have failed conventional treatment
- Necrotizing soft tissue infections where rapid oxygen delivery supports immune function
- Osteomyelitis (bone infections) combined with surgical intervention and antibiotics
- Radiation tissue damage both for prevention and treatment of radiation-induced injuries
- Compromised grafts and flaps in surgical reconstruction
- Sudden sensorineural hearing loss when treated promptly
- Acute thermal burns in specialized cases
These FDA-approved indications represent conditions where randomized controlled trials and extensive clinical experience have established therapeutic benefit. Healthcare providers in Mount Vernon and throughout Washington State can confidently recommend HBOT for these approved uses with documented efficacy.
Scientific Evidence and Research
The scientific foundation for hyperbaric oxygen therapy varies considerably depending on the specific condition. Research published in peer-reviewed journals provides varying levels of evidence for different applications. A systematic review published in the Cochrane Database of Systematic Reviews examining HBOT for diabetic foot ulcers found moderate evidence supporting its use as an adjunctive therapy when combined with standard wound care protocols. The analysis concluded that HBOT significantly increased healing rates in specific patient populations, particularly those with Wagner grade 3 or higher ulcers.
Research from major medical institutions, including those affiliated with the University of California health system, has demonstrated measurable physiological changes during and after hyperbaric oxygen therapy. Studies using advanced imaging techniques show increased blood perfusion in previously compromised tissues and enhanced metabolic activity in healing tissues. Additionally, research examining the immunological effects of HBOT shows improved neutrophil function and enhanced bacterial killing capacity.
However, the scientific community emphasizes that effectiveness varies significantly based on patient selection, underlying pathology, and treatment protocol adherence. Not all patients respond equally to HBOT, and individual factors such as age, comorbid conditions, smoking status, and vascular health influence outcomes. The evidence base is strongest for chronic non-healing wounds and radiation tissue damage, where multiple high-quality studies demonstrate consistent benefit.
When considering how long does physical therapy take, it’s worth noting that HBOT often requires similar commitment timeframes. Both therapies typically demand 20-40 sessions over several weeks for meaningful results.
Off-Label Applications and Claims
Beyond FDA-approved indications, hyperbaric oxygen therapy is sometimes promoted for conditions where evidence remains limited or controversial. These off-label uses require careful scrutiny and should only be pursued under qualified medical supervision. Common off-label applications include:
- Traumatic brain injury and post-concussion syndrome
- Stroke recovery and neurological rehabilitation
- Autism spectrum disorder
- Fibromyalgia and chronic pain conditions
- Multiple sclerosis and other autoimmune conditions
- Sports injuries and athletic recovery
- Lyme disease and tick-borne illnesses
- Aging-related conditions and general wellness
While preliminary research and anecdotal reports suggest potential benefit for some of these conditions, rigorous clinical trials have not yet established clear efficacy. The FDA explicitly cautions against unsubstantiated claims for off-label HBOT uses. Patients considering HBOT for non-approved indications should understand that they’re participating in experimental treatment without guaranteed benefit.
This situation differs from does therapy work in general—where psychological and behavioral therapies have extensive research validation. HBOT’s evidence base for approved uses is strong, but claims beyond those approvals require skepticism and consultation with evidence-based practitioners.
Safety Considerations and Side Effects
Hyperbaric oxygen therapy is generally considered safe when administered in properly equipped facilities by trained medical professionals. However, like all medical treatments, HBOT carries potential risks and side effects that patients should understand:
Common side effects include barotrauma to the ears and sinuses (pressure-related injuries), temporary myopia (nearsightedness) due to lens changes, fatigue following treatment sessions, and claustrophobia in monoplace chambers. These effects are usually mild and resolve quickly.
Serious complications, though rare, can include oxygen toxicity (seizures from excessive oxygen exposure), decompression sickness in extreme cases, and pulmonary complications. Patients with certain conditions—including uncontrolled fever, upper respiratory infections, or a history of thoracic surgery—may face increased risk.
The risk of oxygen toxicity increases with treatment depth and duration, which is why standardized protocols limiting exposure to 90-120 minutes per session have been established. Additionally, patients taking certain medications (particularly chemotherapy agents) may experience increased sensitivity to hyperbaric conditions.
Proper patient screening, medical supervision, and adherence to established protocols minimize these risks substantially. Facilities in Mount Vernon, WA offering HBOT should maintain certification, employ trained hyperbaric technicians, and have emergency protocols in place.
Accessing Hyperbaric Oxygen Therapy in Mount Vernon, WA
Mount Vernon and the surrounding Skagit Valley region have access to hyperbaric oxygen therapy through several medical facilities. Patients seeking HBOT should look for centers accredited by the Undersea and Hyperbaric Medical Society (UHMS) and staffed by certified hyperbaric medicine physicians. When selecting a provider, verify that the facility:
- Maintains current accreditation and certification standards
- Employs board-certified hyperbaric medicine specialists
- Has properly maintained and regularly inspected equipment
- Offers comprehensive patient evaluation and treatment planning
- Provides detailed informed consent documentation
- Has established emergency protocols and trained staff
Before beginning treatment, patients should undergo thorough medical evaluation including pulmonary function testing, baseline hearing assessment (for certain conditions), and psychological screening for claustrophobia. Insurance coverage for HBOT varies depending on whether treatment addresses FDA-approved indications; Medicare and most private insurers cover approved uses but typically deny reimbursement for off-label applications.
Understanding physical therapy cost considerations applies similarly to HBOT expenses. While approved uses may be covered, patients should verify insurance specifics and understand out-of-pocket costs before committing to extended treatment courses.
Comparing HBOT to Other Therapeutic Approaches
Hyperbaric oxygen therapy doesn’t exist in isolation—it’s one of many therapeutic modalities available for various conditions. For chronic wounds, HBOT works synergistically with conventional wound care, vascular interventions, and infection management. For neurological conditions, HBOT might complement physical rehabilitation, occupational therapy, and cognitive training.
The therapy goals you establish with your healthcare provider should guide treatment selection. For approved HBOT indications, the evidence strongly supports its use as an adjunctive therapy. However, for off-label applications, alternative or complementary approaches with stronger evidence bases might be preferable.
Patients interested in comprehensive therapeutic approaches should consult with the MindLift Daily Blog – Therapy Resources for information on complementary psychological and behavioral interventions. Additionally, exploring whether cognitive behavioral therapy for generalized anxiety disorder or other evidence-based therapies might address underlying conditions is valuable.
Research from the National Center for Biotechnology Information demonstrates that multimodal treatment approaches—combining HBOT with conventional therapies—produce superior outcomes compared to monotherapy in many cases.
Frequently Asked Questions
How long does a typical hyperbaric oxygen therapy session last?
Standard HBOT sessions typically last 90 to 120 minutes, including pressurization and depressurization time. The actual breathing of pure oxygen under pressure usually occupies 60-90 minutes. Treatment frequency depends on the condition being treated, ranging from daily sessions to sessions several times weekly.
Is hyperbaric oxygen therapy covered by insurance?
Insurance coverage depends on whether treatment addresses an FDA-approved indication. Medicare and most private insurers cover HBOT for approved conditions when prescribed by qualified physicians. Off-label uses are typically not covered, making them out-of-pocket expenses. Patients should verify coverage with their insurance provider before beginning treatment.
How many treatments are typically needed?
The number of HBOT sessions varies by condition. FDA-approved indications typically require 20-40 treatments, with some conditions requiring up to 60 sessions. Treatment plans are individualized based on patient response, underlying pathology, and clinical progress. Regular reassessment determines whether to continue, modify, or conclude therapy.
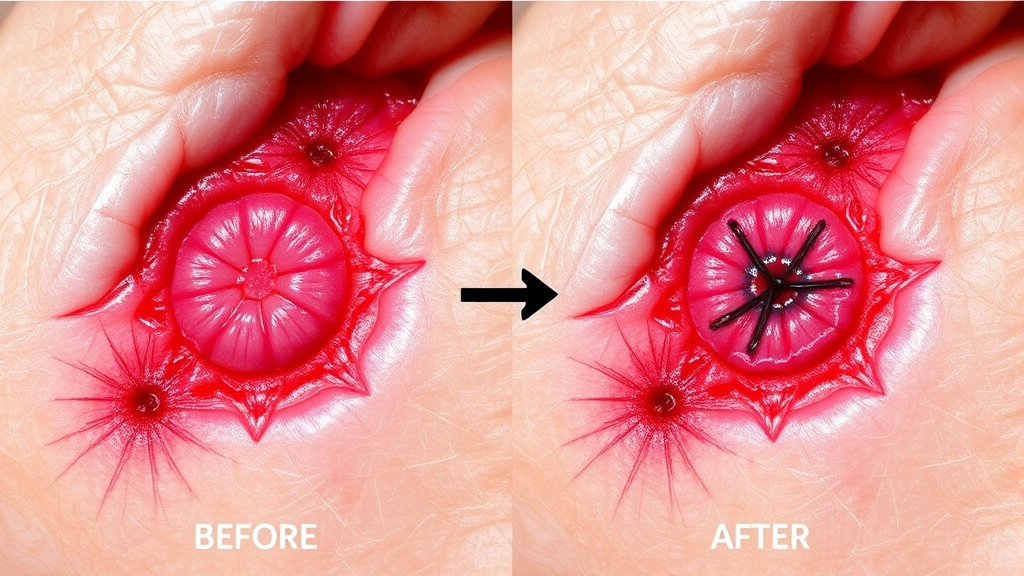
Can hyperbaric oxygen therapy cure chronic wounds?
HBOT significantly improves healing rates for chronic non-healing wounds, particularly diabetic foot ulcers, but it’s not a standalone cure. Rather, it works as an adjunctive therapy alongside wound care, infection management, vascular interventions, and lifestyle modifications. Success requires comprehensive wound care coordination.
Are there contraindications preventing some patients from receiving HBOT?
Yes, certain conditions contraindicate HBOT or increase risk. Uncontrolled high fever, upper respiratory infections, history of thoracic surgery, and untreated pneumothorax are absolute or relative contraindications. Additionally, patients on certain chemotherapy regimens or with uncontrolled claustrophobia may face challenges. Medical evaluation determines individual suitability.
What should I expect during my first hyperbaric oxygen therapy session?
Your first session begins with medical evaluation and education about the pressurization process. You’ll enter the chamber (monoplace or multiplace), and staff will gradually increase pressure while you breathe pure oxygen. You may experience ear pressure similar to airplane descent—equalizing techniques help manage this. Most patients tolerate the process well with proper preparation and instruction.
Can hyperbaric oxygen therapy help with autism or brain injuries?
While some practitioners promote HBOT for autism and traumatic brain injury, evidence remains limited. Some preliminary studies suggest potential benefit, but large-scale randomized controlled trials haven’t established clear efficacy. These applications remain off-label and experimental. Interested patients should discuss evidence limitations with qualified physicians.



