
Hyperbaric Oxygen Therapy: Benefits & Risks Explained
Hyperbaric oxygen therapy (HBOT) has emerged as a compelling treatment modality for various medical conditions, from chronic wounds to decompression sickness. This specialized medical intervention involves exposing patients to pure oxygen in a pressurized chamber, creating an environment where oxygen dissolves into the bloodstream at significantly higher concentrations than would be possible through normal breathing. Whether you’re considering HBOT in Mount Vernon, WA, or simply seeking to understand this therapy better, it’s essential to grasp both its therapeutic potential and inherent risks.
The science behind hyperbaric oxygen therapy is rooted in basic physiology: increased atmospheric pressure allows the lungs to absorb more oxygen, which then saturates the blood plasma and tissues. This enhanced oxygenation can promote healing, reduce inflammation, and support the body’s natural recovery mechanisms. However, like any medical treatment, HBOT comes with considerations and potential adverse effects that patients should understand before beginning treatment.

How Hyperbaric Oxygen Therapy Works
Hyperbaric oxygen therapy operates on the principle of Henry’s Law, which states that the amount of gas dissolved in a liquid is directly proportional to the pressure of that gas above the liquid. During a typical HBOT session, patients enter a pressurized chamber—either monoplace (single occupancy) or multiplace (accommodating multiple patients)—where the atmospheric pressure is increased to between 2.4 and 3.0 atmospheres absolute (ATA).
At sea level, atmospheric pressure is 1 ATA and oxygen comprises 21% of the air we breathe. Inside a hyperbaric chamber operating at 2.8 ATA with 100% oxygen, the partial pressure of oxygen increases dramatically. This allows oxygen to dissolve directly into the blood plasma, bypassing the normal oxygen-carrying capacity of hemoglobin. The result is a substantial increase in oxygen availability to tissues throughout the body.
A standard HBOT session typically lasts 90-120 minutes, during which the chamber is gradually pressurized over about 10-15 minutes, maintaining pressure for the therapeutic period, and then slowly decompressed. Patients often undergo multiple sessions—typically 20-40 treatments over several weeks—depending on their condition and treatment protocol. Understanding how long the effects of hyperbaric oxygen therapy last is crucial for establishing realistic expectations about treatment outcomes.
Primary Medical Applications
The FDA has approved hyperbaric oxygen therapy for 14 specific conditions, though medical practitioners may recommend it for other indications based on emerging research and clinical experience. The approved conditions include:
- Decompression sickness (the bends)
- Air or gas embolism
- Carbon monoxide poisoning
- Chronic osteomyelitis
- Diabetic lower extremity wounds
- Exceptional blood loss anemia
- Necrotizing soft tissue infections
- Radiation tissue injury
- Compromised skin grafts and flaps
- Acute thermal burn injury
- Sudden sensorineural hearing loss
- Idiopathic sudden hearing loss with tinnitus
- Acute cerebral edema
- Chronic wounds of various etiologies
Beyond these FDA-approved indications, researchers are investigating HBOT’s efficacy for conditions including autism spectrum disorder, traumatic brain injury, fibromyalgia, and various post-surgical complications. While preliminary studies show promise, these applications remain investigational and are not universally covered by insurance.
Proven Benefits of HBOT
The therapeutic benefits of hyperbaric oxygen therapy extend across multiple physiological systems. The primary mechanism—enhanced tissue oxygenation—triggers a cascade of beneficial effects that support healing and recovery.
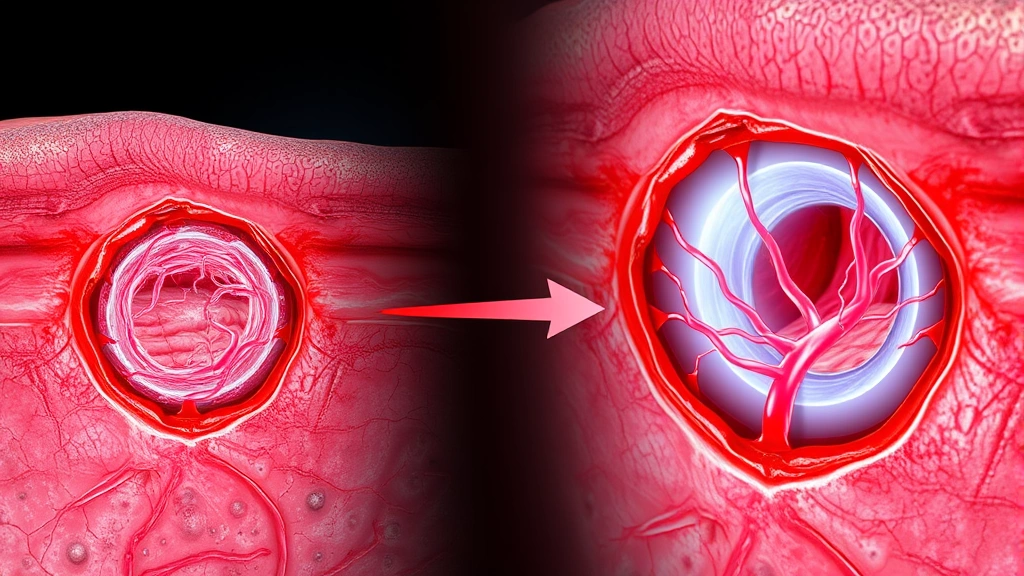
Wound Healing and Tissue Repair: One of the most well-established benefits involves accelerated wound healing, particularly in diabetic foot ulcers and chronic wounds. The increased oxygen availability stimulates angiogenesis (formation of new blood vessels), enhances collagen synthesis, and promotes fibroblast activity. Research published in peer-reviewed medical journals demonstrates that diabetic patients receiving HBOT experience significantly faster wound closure compared to standard care alone.
Infection Control: Enhanced oxygen levels improve the bactericidal activity of white blood cells, particularly neutrophils, which depend on oxygen for their antimicrobial function. This makes HBOT particularly valuable for treating necrotizing soft tissue infections and chronic osteomyelitis, where conventional antibiotics alone may prove insufficient.
Inflammation Reduction: Hyperbaric oxygen therapy modulates inflammatory responses through multiple pathways. While acute inflammation is necessary for healing, chronic inflammation impedes recovery. HBOT helps normalize inflammatory markers and supports the transition from inflammatory to healing phases.
Angiogenesis and Neovascularization: The therapy stimulates the growth of new blood vessels, improving circulation to oxygen-deprived tissues. This is particularly beneficial for patients with compromised vascular function due to diabetes, radiation therapy, or peripheral vascular disease.
Neurological Effects: Emerging evidence suggests HBOT may support neurological recovery by reducing cerebral edema, improving oxygen delivery to damaged neural tissue, and modulating inflammatory responses in the brain.
Potential Risks and Side Effects
While hyperbaric oxygen therapy is generally considered safe when administered properly, patients should be aware of potential complications. Understanding these risks allows for informed decision-making and proper monitoring during treatment.
Barotrauma: Pressure-related injury is the most common complication, typically affecting the middle ear, sinuses, and lungs. During pressurization, patients must equalize pressure in their middle ear by swallowing, yawning, or performing the Valsalva maneuver. Failure to equalize pressure can result in ear pain, hearing loss, or in severe cases, eardrum rupture. Sinus barotrauma presents similarly with sinus pain and congestion. Pulmonary barotrauma, though rare, is the most serious form and occurs when patients hold their breath during decompression, allowing expanding air to rupture lung tissue.
Oxygen Toxicity: Exposure to high partial pressures of oxygen can paradoxically damage tissues through the formation of reactive oxygen species. Central nervous system (CNS) oxygen toxicity may cause seizures, vision changes, nausea, or twitching, typically occurring during or immediately after treatment. Pulmonary oxygen toxicity develops with repeated exposures and presents as chest discomfort, coughing, and reduced vital capacity. These effects are generally reversible when treatments are discontinued.
Claustrophobia and Anxiety: The confined space of a hyperbaric chamber triggers anxiety in some patients. Monoplace chambers, in particular, can provoke claustrophobic responses. Psychological support, pre-treatment orientation, and sometimes anxiolytic medications help manage this issue.
Myopia (Nearsightedness): Temporary changes in lens shape and refractive error occur in approximately 20% of HBOT patients, typically during the initial phase of treatment. This is usually reversible after therapy concludes, though some patients experience permanent mild myopic shift.
Hypoglycemia: Hyperbaric oxygen therapy can increase insulin sensitivity and lower blood glucose levels. Diabetic patients require careful monitoring and may need to adjust medications during treatment courses.
Medication Interactions: Certain medications interact with high-pressure oxygen environments. Doxorubicin and cisplatin, chemotherapy agents, may have altered efficacy. Disulfiram and corticosteroids can increase oxygen toxicity risk. Patients must disclose all medications to their HBOT team.
Treatment Duration and Protocols
The duration and intensity of hyperbaric oxygen therapy vary significantly based on the condition being treated and individual patient factors. Standard protocols typically involve sessions of 90-120 minutes at pressures between 2.4 and 3.0 ATA, conducted five days per week for two to eight weeks.
For diabetic foot ulcers, treatment commonly extends for 20-40 sessions. Acute conditions like carbon monoxide poisoning may require fewer, more intensive treatments. Chronic wounds and radiation injury may necessitate extended courses of 40-60 sessions or more.
The concept of treatment duration and lasting effects is important to discuss with healthcare providers. Some patients experience sustained improvement after completing a course, while others may require periodic maintenance sessions. This depends on the underlying condition, the patient’s overall health status, and their body’s capacity for continued tissue repair and regeneration.
Finding HBOT Services Locally
If you’re seeking hyperbaric oxygen therapy in Mount Vernon, WA, several factors should guide your selection of a treatment facility. Look for centers staffed with board-certified hyperbaric medicine physicians and trained HBOT technicians. Accreditation through organizations like the Undersea and Hyperbaric Medical Society (UHMS) indicates adherence to safety standards and evidence-based practices.
Your primary care physician or specialist can provide referrals to reputable HBOT centers in your region. When evaluating facilities, inquire about their safety protocols, infection control measures, equipment maintenance schedules, and physician credentials. Ask about their experience treating your specific condition and request information about expected outcomes based on their patient population.
Insurance coverage varies significantly depending on your policy and the condition being treated. FDA-approved indications are more likely to be covered, though pre-authorization may be required. Discuss costs, payment options, and insurance requirements during your initial consultation.
Beyond hyperbaric oxygen therapy, consider exploring complementary approaches to healing and recovery. Red light therapy for back pain and other modalities may provide additional therapeutic benefits when combined with HBOT. Additionally, understanding how long physical therapy takes can help you develop a comprehensive rehabilitation timeline if your condition requires multi-modal treatment approaches.
The MindLift Daily Blog offers comprehensive therapy resources and information that can supplement your understanding of various treatment options. When considering whether to pursue HBOT, reviewing whether therapy works for your specific situation helps establish realistic expectations. Understanding therapy cost implications is also essential for comprehensive treatment planning.
Frequently Asked Questions
Is hyperbaric oxygen therapy painful?
HBOT itself is not painful, though ear discomfort may occur if pressure equalization is difficult. Patients should inform their technician immediately if they experience pain during treatment so pressure can be adjusted.
How many sessions are typically needed?
Treatment courses vary from 20-60+ sessions depending on the condition. Your physician will establish a specific protocol based on your diagnosis, severity, and response to initial treatments.
Are there any contraindications to HBOT?
Untreated pneumothorax (collapsed lung) is an absolute contraindication. Patients with fever, upper respiratory infections, or certain medications should discuss potential risks with their physician before treatment begins.
Can children receive hyperbaric oxygen therapy?
Yes, children can undergo HBOT when medically indicated. Treatment protocols may be modified for younger patients, and parental presence in multiplace chambers is often permitted.
How quickly will I see results?
Results vary by condition. Some patients notice improvements within several sessions, while others require weeks of treatment before significant changes become apparent. Chronic conditions typically require longer treatment courses than acute presentations.
Is HBOT covered by insurance?
FDA-approved indications are often covered by insurance, though pre-authorization is typically required. Coverage varies significantly by policy and carrier. Contact your insurance provider for specific information about your plan.
What should I do to prepare for HBOT?
Avoid caffeine and alcohol before treatment, wear comfortable cotton clothing, and avoid applying lotions or oils to your skin. Follow all pre-treatment instructions provided by your HBOT facility.



