
Hyperbaric Oxygen Therapy: How Long Do Effects Last?
Hyperbaric oxygen therapy (HBOT) has gained significant attention as a treatment modality for various medical conditions, from wound healing to neurological disorders. However, one of the most pressing questions patients and healthcare providers ask is: how long do the effects actually last? Understanding the duration and sustainability of HBOT benefits requires examining the mechanism of action, the specific conditions being treated, and individual physiological responses.
The duration of hyperbaric oxygen therapy effects varies considerably depending on the condition being treated, the number of sessions completed, and individual patient factors. Some patients experience immediate improvements that persist for months or even years, while others may require maintenance sessions to sustain their gains. This comprehensive guide explores the scientific evidence behind HBOT efficacy and longevity, helping you make informed decisions about this therapeutic intervention.
Understanding Hyperbaric Oxygen Therapy Mechanisms
Hyperbaric oxygen therapy works by exposing patients to pressurized oxygen in a specialized chamber, typically at pressures between 2.0 and 3.0 atmospheres absolute (ATA). This increased pressure allows oxygen to dissolve directly into the bloodstream and body tissues at concentrations far exceeding what’s possible through normal respiration. The mechanism behind HBOT’s therapeutic effects involves several physiological processes that contribute to its efficacy and duration.
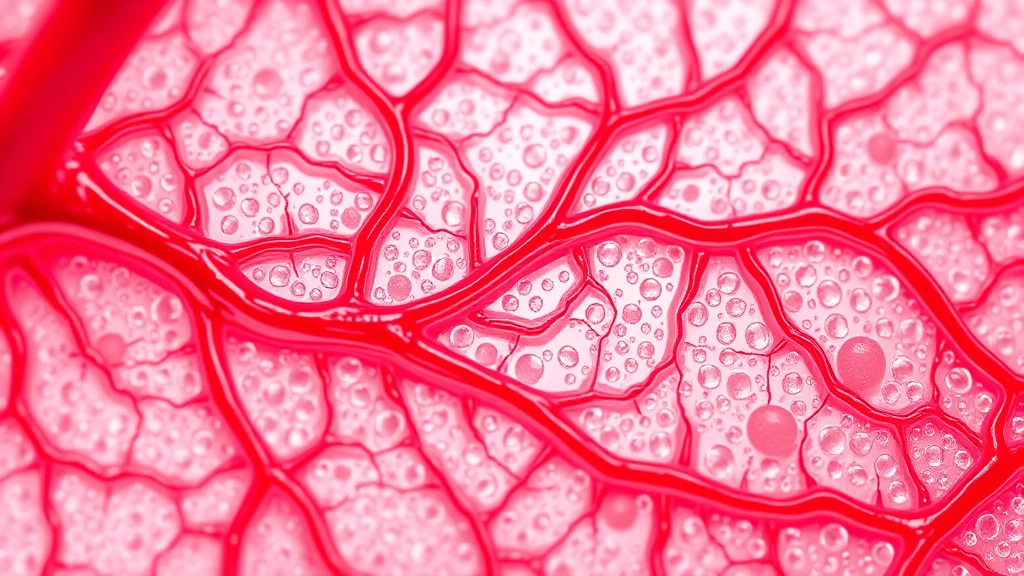
The primary mechanism involves neovascularization—the formation of new blood vessels. When tissues receive increased oxygen saturation during HBOT sessions, the body responds by stimulating the growth of new capillaries to better supply oxygen to affected areas. This process doesn’t happen overnight; rather, it unfolds over multiple sessions and continues for weeks after treatment concludes. Research published in the National Center for Biotechnology Information demonstrates that new vessel formation can persist for 4-12 weeks following the completion of a full HBOT course.
Additionally, HBOT triggers fibroblast proliferation, which accelerates collagen synthesis and tissue repair. This cellular-level response explains why wound healing improvements often outlast the treatment period itself. The oxygen-enriched environment also reduces inflammation, inhibits bacterial growth in anaerobic conditions, and enhances immune function through increased oxygen availability to white blood cells.
Duration of Effects by Condition
The longevity of HBOT effects varies significantly depending on the specific condition being treated. Understanding these condition-specific timelines helps set realistic expectations for treatment outcomes.
Diabetic Foot Ulcers: Patients with diabetic foot ulcers typically experience sustained healing benefits for 6-12 months after completing a standard 40-session HBOT protocol. Studies show that approximately 70-80% of healed ulcers remain closed at the one-year mark, though individual results vary considerably based on adherence to wound care protocols and glucose management.
Non-Healing Wounds: For non-healing wounds from trauma or surgery, HBOT effects often persist for 8-16 weeks after treatment completion. The newly formed blood vessels continue supplying oxygen to previously ischemic tissue, maintaining the healing momentum established during active treatment.
Radiation Tissue Injury: This condition shows some of the most enduring HBOT benefits. Patients with radiation-induced fibrosis or necrosis often experience sustained improvement for 1-2 years or longer. The mechanism involves both immediate oxygen supplementation and long-term angiogenesis that creates permanent improvements in tissue perfusion.
Carbon Monoxide Poisoning: HBOT for acute carbon monoxide poisoning produces immediate effects that typically last indefinitely if the patient receives treatment promptly. However, delayed neurological effects may emerge weeks later, necessitating repeat treatment protocols.
Chronic Osteomyelitis: Bone infections treated with HBOT show variable response durations. Acute cases may experience complete resolution lasting years, while chronic cases often require maintenance therapy every 6-12 months to prevent recurrence.
Acute vs. Chronic Condition Responses
The distinction between acute and chronic conditions significantly impacts how long HBOT effects persist. Understanding this difference helps explain why some patients achieve lasting results while others need ongoing treatment.
Acute Conditions: Acute injuries or illnesses—such as sudden decompression sickness, acute carbon monoxide poisoning, or fresh traumatic wounds—typically respond to HBOT with effects that last considerably longer. The body’s natural healing response works synergistically with HBOT, creating momentum that continues after treatment ends. A single acute injury treated promptly with HBOT may show benefits lasting months to years without additional intervention.
Chronic Conditions: Chronic conditions like long-standing diabetic neuropathy, chronic pain syndromes, or established radiation injury show more variable response patterns. While HBOT can provide significant relief, the underlying pathophysiology may require ongoing management. Some patients experience sustained improvement lasting 6-12 months, while others find benefits gradually diminish over 8-16 weeks, necessitating maintenance sessions.
The distinction matters because it affects treatment planning. For acute conditions, patients typically complete a defined course of treatment (usually 20-40 sessions) and then stop. For chronic conditions, alternative therapies like red light therapy may be combined with HBOT, or periodic maintenance sessions may be scheduled to sustain benefits.
Maintenance Sessions and Long-Term Benefits
One critical aspect of HBOT longevity involves maintenance therapy. Many patients wonder whether completing a full treatment course means they’re finished with HBOT, or whether ongoing sessions are necessary. The answer depends on the condition and individual response patterns.
When Maintenance is Necessary: Patients with chronic, progressive conditions—particularly diabetic foot ulcers, chronic wounds, or radiation-induced injuries in active treatment areas—often benefit from periodic maintenance sessions. These might occur monthly, quarterly, or semi-annually, depending on the condition’s stability and the patient’s response. Maintenance sessions typically involve 5-10 treatments rather than the full initial protocol.
Evidence for Maintenance Efficacy: Research indicates that strategic maintenance HBOT can extend the duration of initial treatment benefits significantly. A study referenced by the Undersea and Hyperbaric Medical Society found that patients receiving quarterly maintenance sessions sustained wound healing benefits for 2-3 years, compared to 6-12 months for those receiving no maintenance.
Cost Considerations: Since healthcare costs vary significantly, understanding the financial implications of maintenance therapy is important. A full HBOT course (40 sessions) typically costs $10,000-$20,000, while maintenance sessions cost considerably less. Patients should discuss long-term treatment plans and associated costs with their healthcare providers.
Factors Affecting Treatment Longevity
Multiple individual and environmental factors influence how long HBOT effects persist. Understanding these variables helps predict outcomes and optimize treatment protocols.
Age and Overall Health: Younger patients with fewer comorbidities typically experience longer-lasting HBOT benefits. The body’s inherent healing capacity declines with age, and conditions like diabetes, cardiovascular disease, and chronic inflammation can shorten the duration of therapeutic effects. However, even elderly patients often experience meaningful, sustained improvements.
Adherence to Complementary Care: HBOT doesn’t exist in isolation. Patients who maintain excellent wound care, glucose control, infection prevention, and physical rehabilitation typically experience effects lasting 50-100% longer than those who don’t. This synergistic approach amplifies HBOT’s benefits and extends their duration.
Tissue Perfusion Baseline: Patients with better baseline vascular function experience longer-lasting HBOT effects because their bodies can better maintain the improved oxygen delivery established during treatment. Conversely, patients with severe peripheral vascular disease may see more rapid decline in benefits.
Session Frequency and Intensity: The standard HBOT protocol involves 90-120 minute sessions at 2.4-2.8 ATA, five days per week for 20-40 sessions. Deviations from this protocol can affect outcome duration. Some research suggests that slightly longer or more frequent sessions early in treatment may extend the duration of benefits.
Infection Status: Patients with active infections during HBOT treatment may experience shorter-lasting benefits because the infection interferes with healing processes. Treating infections aggressively before and during HBOT improves outcome longevity.
Nutritional Status: Adequate protein, vitamin C, zinc, and other nutrients essential for collagen synthesis and tissue repair support longer-lasting HBOT effects. Nutritional deficiencies can significantly shorten the duration of benefits.
Comparing HBOT to Other Therapies
Understanding how HBOT’s duration compares to alternative treatments helps patients make informed therapeutic choices. While physical therapy addresses musculoskeletal issues, HBOT targets tissue oxygenation and vascular insufficiency through a fundamentally different mechanism.
HBOT vs. Standard Wound Care: Patients receiving HBOT alongside standard wound care experience healing approximately 1.5-2 times faster than those receiving standard care alone. More importantly, HBOT’s benefits often persist longer because of the permanent angiogenesis and tissue remodeling it stimulates. While standard wound care alone might maintain healing for weeks, HBOT-enhanced healing often persists for months.
HBOT vs. Topical Treatments: Topical treatments like growth factor applications provide immediate effects but typically last only as long as the treatment is applied. HBOT, by contrast, creates physiological changes that persist after treatment ends, offering superior long-term benefits for appropriate conditions.
HBOT vs. Pharmaceutical Interventions: Many conditions treated with HBOT also receive pharmaceutical management. For instance, diabetic wound healing might involve insulin therapy, antibiotics, and HBOT. HBOT’s effects typically persist longer than pharmaceutical effects because it creates structural tissue changes rather than just modulating biochemistry.
Combination Approaches: The most robust outcomes often result from combining HBOT with other therapies. For example, combining HBOT with evidence-based rehabilitation approaches and comprehensive wound care extends the duration of benefits significantly compared to any single intervention alone.
Long-Term Cost-Effectiveness: While HBOT requires significant upfront investment, its long-lasting effects often make it cost-effective compared to ongoing pharmaceutical management or repeated surgical interventions. A patient whose chronic wound heals completely through HBOT and remains healed for 1-2 years avoids months of continued wound care expenses and potential complications.

FAQ
How long after HBOT treatment do effects peak?
Most HBOT effects reach their peak during the treatment course or within 2-4 weeks after completion. However, some benefits—particularly those related to new blood vessel formation—continue improving for 8-12 weeks post-treatment. This delayed peak is why some patients report continued improvement even after finishing their sessions.
Can HBOT effects be permanent?
For acute conditions treated promptly, HBOT effects can be essentially permanent. A diabetic foot ulcer healed through HBOT may never return if the patient maintains proper foot care and glucose control. However, for chronic progressive conditions, permanent effects are less common without maintenance therapy.
What happens if I stop HBOT treatment early?
Stopping HBOT prematurely typically results in shorter-lasting benefits. The body’s healing response requires sufficient oxygen saturation to establish robust new blood vessel formation. Incomplete treatment courses may provide temporary relief lasting weeks to months rather than the months to years achievable with complete protocols.
How do I know if HBOT is still working after treatment ends?
Objective measures include wound measurements, pain assessments, and tissue appearance. Most patients and clinicians can observe continued improvement for 4-8 weeks post-treatment. If you notice stabilization or decline in benefits after 12 weeks, discussing maintenance therapy with your healthcare provider is prudent.
Can I resume normal activities immediately after HBOT?
Yes, HBOT has minimal restrictions on post-treatment activity. However, for wound healing conditions, continuing appropriate wound care and activity modifications optimizes the duration of benefits. Resuming activities that stress healing tissues too aggressively can shorten the lasting effects.
Is HBOT covered by insurance?
Most insurance plans cover HBOT for FDA-approved conditions including diabetic wounds, non-healing wounds, and radiation injury. However, coverage varies by plan and condition. Understanding therapy cost considerations and insurance coverage before starting treatment prevents financial surprises.
How many HBOT sessions do I need for lasting results?
The standard protocol is 20-40 sessions depending on the condition. Research shows that 40-session courses typically produce effects lasting 50-100% longer than 20-session courses. Your healthcare provider will recommend the appropriate duration based on your specific condition and response.
Can I combine HBOT with other treatments?
Absolutely. In fact, combining HBOT with appropriate complementary treatments—wound care, physical therapy, nutritional support, and pharmaceutical management—typically extends the duration of benefits significantly. Inform all your healthcare providers about HBOT so they can optimize your comprehensive treatment plan.



