Therapy for Gum Recession: Expert Insights and Supportive Treatment Options
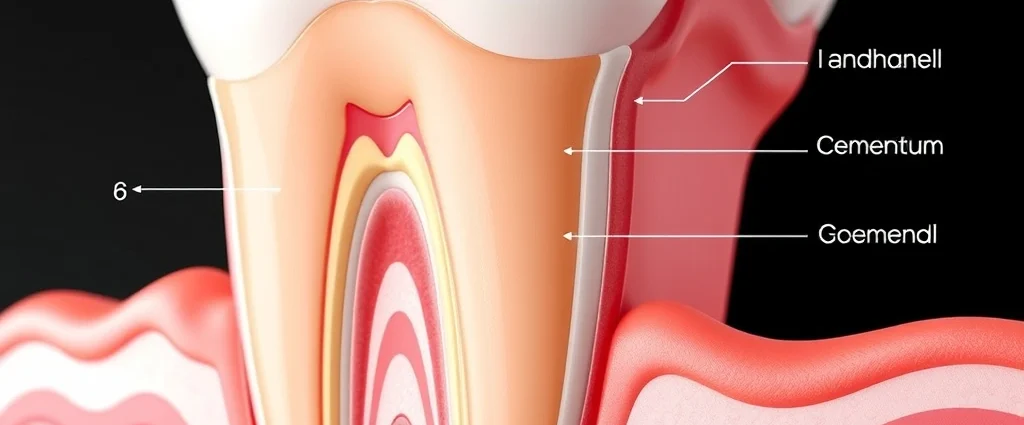
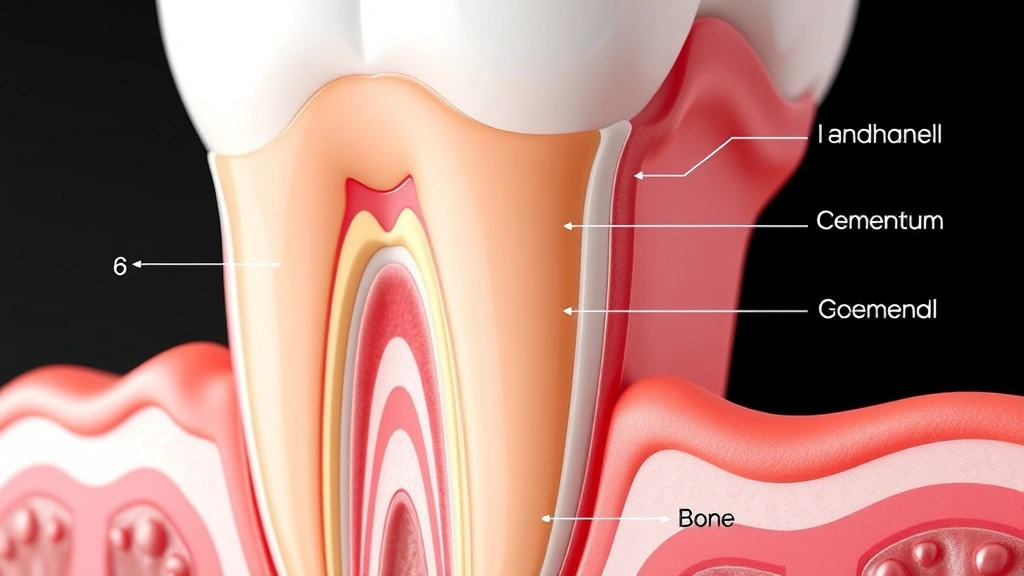
Gingival recession, commonly known as gum recession, affects millions of individuals worldwide and represents one of the most prevalent periodontal concerns in modern dentistry. This condition occurs when the gum tissue surrounding teeth gradually wears away or pulls back, exposing the tooth root beneath. While gum recession may seem like a purely cosmetic issue, it carries significant implications for oral health, including increased sensitivity, root decay, and potential tooth loss if left untreated. Understanding the mechanisms behind gum recession and the various therapeutic interventions available is essential for patients seeking to preserve their dental health and maintain an aesthetically pleasing smile.
Supportive therapy for gingival recession encompasses a comprehensive range of interventions, from non-invasive preventive measures to advanced surgical techniques. The approach to treatment depends on the severity of recession, the underlying causative factors, and individual patient circumstances. Modern dentistry emphasizes early intervention and patient education as cornerstone elements of successful gum recession management, recognizing that prevention and early detection significantly improve outcomes and reduce the need for extensive surgical procedures.

Understanding Gingival Recession: Causes and Risk Factors
Gum recession develops through multiple interconnected mechanisms, with mechanical trauma and inflammatory processes being primary contributors. Aggressive tooth brushing remains one of the most common preventable causes, as excessive force and improper technique can gradually erode gingival tissue and underlying bone structure. The American Dental Association recommends using a soft-bristled toothbrush with gentle circular motions to minimize mechanical damage while maintaining effective plaque removal.
Periodontal disease represents another significant causative factor, where bacterial infection and subsequent inflammation trigger progressive destruction of gingival and periodontal tissues. Patients with untreated gingivitis or periodontitis experience accelerated gum recession as the inflammatory process compromises tissue integrity. Additionally, genetic predisposition plays a crucial role, with some individuals inheriting naturally thin or fragile gingival tissue that predisposes them to recession regardless of oral hygiene practices.
Tobacco use significantly accelerates gum recession through multiple pathways, including impaired immune function, reduced blood flow, and direct chemical damage to gingival tissues. Smoking compromises the body’s ability to heal and maintain healthy periodontal structures, making smokers substantially more vulnerable to severe recession. Hormonal fluctuations during pregnancy, menopause, and hormonal contraceptive use can also increase recession risk by altering gingival tissue composition and inflammatory response patterns.
Orthodontic treatment, while providing aesthetic and functional benefits, occasionally contributes to gum recession when teeth are moved beyond the alveolar bone envelope. Proper treatment planning and monitoring during orthodontics help minimize this risk. Occlusal trauma from excessive bite forces, misalignment, or bruxism can similarly accelerate recession by creating mechanical stress on gingival tissues.

Clinical Assessment and Diagnosis
Accurate diagnosis of gingival recession requires comprehensive clinical examination using standardized measurement techniques. Dentists employ the Miller Classification system, which categorizes recession severity into four classes based on the extent of gingival loss and the relationship to the mucogingival junction. This classification helps guide treatment planning and predict prognosis for surgical root coverage procedures.
Probing depth measurements, clinical attachment level assessment, and visual examination of the recession site provide essential diagnostic information. Radiographic imaging helps identify bone loss patterns and assess the extent of root exposure. Modern digital periodontal probes offer precise measurements, enabling practitioners to monitor recession progression over time and evaluate treatment efficacy.
Comprehensive medical and dental history assessment identifies contributing factors and helps prioritize interventions. Patients should disclose tobacco use, stress levels, medications, and oral hygiene practices, as these factors significantly influence recession development and treatment outcomes. Understanding the patient’s specific risk profile enables clinicians to develop personalized treatment strategies addressing underlying causative factors.
Non-Surgical Supportive Therapy Approaches
Non-surgical interventions form the foundation of gingival recession management and prove effective for mild to moderate cases. The primary objective involves halting recession progression and creating conditions favorable for tissue regeneration. Comprehensive therapy resources emphasize the importance of patient compliance with recommended protocols.
Mechanical Plaque Control and Oral Hygiene Modification represents the cornerstone of non-surgical therapy. Patients must transition from aggressive brushing techniques to gentle, methodical approaches using soft-bristled toothbrushes. The Bass technique, involving gentle vibration at the gingival margin, effectively removes plaque while minimizing tissue trauma. Electric toothbrushes with pressure-limiting features provide additional safety, particularly for patients prone to aggressive brushing.
Interdental cleaning using floss or interdental brushes removes biofilm from areas inaccessible to toothbrushes. However, technique is critical—aggressive flossing can accelerate recession, particularly in patients with existing gingival compromise. Water irrigation devices offer gentler alternatives for patients with sensitive or recessed areas.
Antimicrobial and Anti-inflammatory Therapy addresses the inflammatory component of recession, particularly in periodontally compromised patients. Chlorhexidine rinses reduce bacterial load and inflammation, though prolonged use carries risks of staining and disrupted oral microbiome. Newer antimicrobial agents, including essential oil-based products, provide alternatives with potentially fewer adverse effects.
Topical fluoride applications strengthen exposed root surfaces and reduce sensitivity by occluding dentinal tubules. Professional fluoride treatments, applied by dental professionals, deliver higher concentrations than over-the-counter products. Desensitizing toothpastes containing potassium nitrate or arginine provide symptomatic relief for patients experiencing root sensitivity.
Smoking Cessation and Lifestyle Modification significantly impact recession progression and treatment success. Patients who quit smoking experience improved healing capacity and reduced inflammation. Stress management techniques may help patients with stress-related bruxism or aggressive clenching behaviors that contribute to recession.
Surgical Interventions for Advanced Recession
Surgical therapy becomes necessary when non-surgical approaches fail to arrest recession or when aesthetic and functional concerns warrant intervention. Multiple surgical techniques exist, each with specific indications, advantages, and limitations.
Free Gingival Graft (FGG) represents one of the oldest and most predictable surgical approaches. This technique involves harvesting keratinized tissue from the palate and suturing it to the recession site. While highly successful for root coverage, FGG creates a secondary surgical site and may result in color discrepancies between grafted and native tissue. The procedure works particularly well for patients requiring increased keratinized gingival width in addition to recession coverage.
Connective Tissue Graft (CTG) has become increasingly popular due to superior aesthetic outcomes compared to FGG. This technique involves harvesting subepithelial connective tissue from the palate while preserving the overlying epithelium, then positioning it beneath a partial-thickness flap at the recession site. The overlying tissue maintains native coloration and texture, providing more natural-appearing results. Success rates for complete root coverage typically exceed 80-90% with CTG.
Coronally Advanced Flap (CAF) utilizes the patient’s existing gingival tissue, eliminating the need for donor site grafting. This technique involves creating a partial-thickness flap and advancing it coronally to cover the exposed root. CAF works best for shallow to moderate recession with adequate gingival tissue available for advancement. When combined with connective tissue grafts, CAF improves outcomes for more extensive defects.
Guided Tissue Regeneration (GTR) employs biocompatible membranes to direct tissue healing and promote periodontal regeneration. Membranes create space for periodontal ligament and bone regeneration while excluding epithelial tissue. GTR shows promise for treating recession with concurrent periodontal defects, though outcomes depend on proper case selection and technique execution.
Soft Tissue Augmentation with Biomaterials represents an emerging approach utilizing xenografts, allografts, or synthetic biomaterials to enhance graft volume and improve outcomes. Products containing acellular dermal matrix or collagen provide scaffold structures that facilitate tissue integration. These materials reduce patient morbidity by eliminating palatal donor site harvesting, though they carry higher costs compared to autogenous grafts.
Professional Management and Long-Term Care
Successful gum recession management requires ongoing professional oversight and patient partnership. Regular periodontal evaluations, typically every three to six months depending on severity and risk factors, monitor recession progression and treatment response. Professional prophylaxis removes calculus and biofilm from exposed root surfaces, which are more susceptible to decay than normal tooth surfaces.
Root surface debridement removes cementum and dentin damaged by caries or trauma, creating a clean surface favorable for attachment and healing. Laser-assisted debridement offers enhanced precision and reduced tissue trauma compared to conventional instrumentation. Specialized therapy approaches for different populations underscore the importance of tailored care strategies.
Bite force assessment and occlusal adjustment address traumatic occlusion contributing to recession. Selective grinding, orthodontic repositioning, or restorative correction may be necessary to eliminate excessive forces on compromised tissues. For patients with bruxism or clenching habits, nightguards distribute forces more favorably and protect grafted tissues during healing.
Patient Education and Prevention Strategies
Patient education represents a critical yet often underutilized component of recession management. Comprehensive instruction regarding proper oral hygiene techniques, with demonstration and practice, significantly improves compliance and outcomes. Visual aids, including intraoral photographs showing recession progression or improvement, motivate patients to maintain recommended protocols.
Dietary counseling addressing acidic food and beverage consumption helps prevent additional root surface damage. Acidic exposures from citrus fruits, sports drinks, and carbonated beverages demineralize exposed root surfaces, accelerating decay. Patients should rinse with water after acidic exposures and wait 30 minutes before brushing to avoid abrading softened enamel and cementum.
Stress management education helps patients with stress-related parafunctional habits. Recognizing bruxism or clenching triggers and implementing relaxation techniques, including meditation or progressive muscle relaxation, reduce destructive bite forces. Occupational therapy principles, as discussed in occupational therapy resources, can inform stress reduction strategies.
Tobacco cessation programs provide essential support for patients motivated to quit smoking. Combining behavioral counseling with pharmacologic aids, including nicotine replacement therapy or prescription medications, significantly improves cessation rates. Dental professionals should actively discuss smoking’s impact on periodontal health and support patients throughout the cessation process.
Emerging Technologies in Recession Treatment
Regenerative medicine approaches utilizing stem cells and growth factors represent the frontier of gum recession therapy. Platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) concentrate growth factors and cellular elements that promote healing and tissue regeneration. When combined with surgical flap procedures or used alone, these autologous products enhance outcomes without introducing foreign materials.
Enamel matrix derivatives (EMD) stimulate periodontal regeneration by mimicking the biological signals present during tooth development. Applied to surgical sites, EMD promotes cementum formation, periodontal ligament regeneration, and alveolar bone healing. Research demonstrates that EMD-augmented procedures achieve superior outcomes compared to conventional techniques, particularly for extensive recession defects.
Recent clinical studies demonstrate the efficacy of acellular dermal matrix allografts in achieving predictable root coverage with minimal patient morbidity. These materials eliminate the need for donor site harvesting while providing scaffold structures that facilitate tissue integration and regeneration. Long-term follow-up data confirm stability of coverage and patient satisfaction with aesthetic outcomes.
Three-dimensional imaging technologies, including cone beam computed tomography (CBCT), provide detailed visualization of bone architecture and soft tissue dimensions. Advanced imaging guides surgical planning, helping clinicians optimize graft positioning and predict treatment success. Digital surgical guides, derived from CBCT data, enhance surgical precision and reproducibility.
Laser-assisted therapies, including Er:YAG and Nd:YAG lasers, offer minimally invasive alternatives for gum recession treatment. Lasers promote hemostasis, reduce postoperative inflammation, and may stimulate tissue regeneration through photobiomodulation effects. PubMed Central contains numerous studies evaluating laser efficacy for periodontal applications.
Artificial intelligence and machine learning algorithms increasingly assist in periodontal diagnosis and treatment planning. These technologies analyze radiographic images and clinical data to identify recession patterns, predict progression, and recommend personalized treatment approaches. As artificial intelligence capabilities expand, clinical decision support systems will enhance diagnostic accuracy and optimize treatment selection.
Telemedicine platforms enable remote periodontal consultations, expanding access to specialized care. Patients in underserved areas can receive expert guidance on recession management without traveling to specialized clinics. Digital photography and intraoral scanning facilitate remote assessment, though in-person evaluation remains necessary for definitive diagnosis and surgical planning.
The integration of supportive therapy approaches with emerging technologies represents the future of gum recession management. Personalized medicine principles, considering individual genetic, environmental, and behavioral factors, will enable clinicians to develop optimized treatment plans maximizing success rates while minimizing morbidity. Continued research and clinical innovation promise even more effective and minimally invasive interventions for this common and consequential dental condition.
Understanding that comprehensive therapy approaches extend across multiple health domains, dental professionals should recognize the interconnections between oral health and systemic well-being. Patients seeking treatment should discuss their specific circumstances with qualified periodontists or general dentists experienced in recession management to determine the most appropriate therapeutic strategy.
FAQ
What is gingival recession and why does it occur?
Gingival recession occurs when gum tissue gradually wears away or pulls back from teeth, exposing tooth roots. Common causes include aggressive tooth brushing, periodontal disease, tobacco use, genetic predisposition, hormonal changes, orthodontic treatment, and occlusal trauma. Understanding your specific risk factors helps determine appropriate preventive and therapeutic measures.
Can gum recession be reversed without surgery?
Mild to moderate gum recession may stabilize or improve with non-surgical supportive therapy, including improved oral hygiene, antimicrobial treatment, fluoride applications, and lifestyle modifications. However, surgical intervention typically provides superior outcomes for significant root coverage, particularly in extensive recession cases.
What are the most predictable surgical techniques for treating gum recession?
Connective tissue grafts and free gingival grafts demonstrate the highest success rates for root coverage, with studies reporting complete coverage in 80-90% of cases. Coronally advanced flaps work well for shallow to moderate recession with adequate gingival tissue. The optimal technique depends on recession severity, tissue availability, and aesthetic considerations.
How long does recovery take after gum graft surgery?
Initial healing typically occurs within 2-3 weeks, though complete tissue maturation and remodeling continue for 6-12 months. Patients must follow strict postoperative instructions, including activity restrictions, dietary modifications, and meticulous oral hygiene using prescribed rinses rather than mechanical cleaning during the initial healing period.
What is the relationship between gum recession and tooth sensitivity?
Exposed tooth roots lack protective enamel and contain numerous open dentinal tubules leading to the tooth’s nerve. This anatomical exposure causes heightened sensitivity to temperature, pressure, and tactile stimuli. Desensitizing treatments and protective measures help manage sensitivity while addressing underlying recession.
How can I prevent gum recession?
Prevention involves using soft-bristled toothbrushes with gentle technique, maintaining excellent oral hygiene, controlling periodontal disease through professional care, quitting tobacco use, managing stress-related clenching, and addressing occlusal trauma. Regular dental evaluations identify early recession, enabling timely intervention before significant damage occurs.
Does insurance cover gum recession treatment?
Coverage varies significantly based on insurance plans and whether treatment is deemed medically necessary versus cosmetic. Non-surgical supportive therapy typically receives better coverage than surgical procedures. Patients should discuss coverage with their insurance providers and dental offices, as many clinicians offer treatment plans accommodating various financial circumstances.
Are there risks associated with gum graft surgery?
All surgical procedures carry inherent risks, including infection, bleeding, and adverse reactions to anesthesia. Graft-specific complications include graft failure, inadequate root coverage, and donor site morbidity. Choosing experienced periodontists, following postoperative instructions carefully, and maintaining excellent oral hygiene minimize complications. Research on therapy effectiveness emphasizes the importance of qualified providers and patient compliance.