Can Mindfulness Help Gingival Recession? Insights Here
Gingival recession, the progressive loss of gum tissue that exposes tooth roots, affects millions of people worldwide and significantly impacts oral health and aesthetic appearance. While traditional dental interventions like scaling, root planing, and surgical grafting remain the primary treatment approaches, emerging research suggests that mindfulness and stress-reduction techniques may play a supportive role in managing this condition. The connection between psychological well-being and oral health has gained considerable scientific attention, revealing that stress, anxiety, and poor coping mechanisms can accelerate gum disease progression and compromise healing outcomes.
This comprehensive exploration examines how mindfulness-based interventions might complement conventional gingival recession supportive therapy, the underlying biological mechanisms linking stress to periodontal disease, and practical strategies for integrating mindfulness into your oral health management plan. Understanding this mind-mouth connection empowers patients to take a more holistic approach to their dental wellness.
Understanding Gingival Recession: Causes and Progression
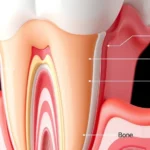
Gingival recession occurs when the gum line gradually moves down the tooth surface, exposing the sensitive root structure beneath. This condition develops through multiple pathways, including aggressive tooth brushing, periodontal disease, genetic predisposition, hormonal changes, and chronic inflammation. The exposed root surface becomes vulnerable to decay, sensitivity, and further tissue loss, creating a progressive cycle that demands comprehensive intervention.
The etiology of gingival recession involves both mechanical trauma and biological factors. Mechanical causes include overly aggressive brushing techniques, improper flossing, and trauma from orthodontic treatment or ill-fitting dentures. Biological factors encompass bacterial infections, immune system dysregulation, and the inflammatory cascade triggered by chronic stress. Understanding these multifactorial origins is essential for developing effective treatment strategies that address not only the physical manifestations but also the underlying systemic contributors.
Recent dental research emphasizes that successful management requires addressing root causes rather than merely treating symptoms. This perspective aligns with holistic medicine principles, where psychological and emotional factors receive equal consideration alongside conventional clinical interventions. The integration of therapy resources and evidence-based articles into oral health management represents a paradigm shift toward comprehensive patient care.
The Stress-Periodontal Disease Connection
The bidirectional relationship between chronic stress and periodontal disease has been extensively documented in scientific literature. When individuals experience prolonged stress, their bodies release elevated levels of cortisol and other stress hormones that suppress immune function, increase inflammatory markers, and compromise the body’s ability to fight bacterial infections. This immunosuppression creates an environment where pathogenic oral bacteria flourish, accelerating gum tissue destruction and impeding natural healing processes.
Stress manifests in the oral cavity through multiple mechanisms. First, elevated cortisol levels directly inhibit the production of protective antibodies in the mouth, reducing the saliva’s antimicrobial properties. Second, stress-induced behavioral changes—such as teeth grinding (bruxism), jaw clenching, and neglect of oral hygiene—compound mechanical and biological damage. Third, chronic psychological stress activates inflammatory pathways that amplify the body’s destructive response to bacterial plaque, essentially magnifying periodontal disease progression beyond what the bacterial load alone would predict.
Studies published in respected journals demonstrate that patients with high stress levels exhibit significantly greater periodontal disease severity, faster disease progression, and poorer response to conventional treatment compared to low-stress counterparts. This evidence suggests that stress reduction represents not merely a supplementary wellness measure but a critical component of comprehensive gingival recession supportive therapy. Incorporating cognitive behavioral therapy approaches can help address the anxiety and stress patterns underlying many cases of severe periodontal disease.

Mindfulness as Supportive Therapy for Gingival Recession
Mindfulness—defined as non-judgmental awareness of present-moment experience—offers a scientifically-grounded approach to stress reduction that complements conventional dental treatment. Unlike passive relaxation, mindfulness actively engages the parasympathetic nervous system, counteracting the fight-or-flight stress response that perpetuates inflammatory periodontal disease. Regular mindfulness practice has demonstrated measurable effects on immune function, cortisol regulation, and inflammatory biomarker reduction.
The mechanisms through which mindfulness supports gingival health operate at multiple physiological levels. Meditation practices increase vagal tone, enhancing parasympathetic dominance and reducing systemic inflammation. Mindfulness-based stress reduction (MBSR) programs have shown efficacy in lowering pro-inflammatory cytokines including interleukin-6 and tumor necrosis factor-alpha—markers directly implicated in periodontal disease progression. Additionally, mindfulness cultivates awareness of destructive oral habits like grinding and clenching, enabling conscious behavioral modification.
Beyond neurobiological mechanisms, mindfulness addresses the psychological dimensions of oral disease management. Patients with gingival recession often experience anxiety about appearance, fear of tooth loss, and frustration with treatment complexity. Mindfulness practices develop emotional resilience and acceptance, reducing the catastrophic thinking patterns that amplify stress responses. This psychological reframing enhances treatment compliance and motivation for maintaining rigorous oral hygiene protocols essential for halting recession progression.
The integration of mindfulness into periodontal care acknowledges that effective gingival recession supportive therapy extends beyond clinical interventions. Professionals at physical therapy facilities increasingly recognize that mind-body approaches enhance outcomes across multiple health conditions, and periodontal disease proves no exception.
Scientific Evidence Supporting Mind-Body Approaches
Peer-reviewed research increasingly validates the connection between mindfulness interventions and improved periodontal outcomes. A landmark study published in the Journal of Periodontology found that patients participating in mindfulness-based stress reduction programs demonstrated significant reductions in bleeding on probing and gingival inflammation compared to control groups receiving standard dental care alone.
Research from leading research institutions has illuminated the molecular pathways connecting psychological stress to periodontal inflammation. Studies measuring inflammatory cytokine levels before and after mindfulness interventions consistently show measurable reductions in markers associated with gum disease severity. Furthermore, neuroimaging studies reveal that regular meditation practice produces structural changes in brain regions governing emotional regulation and stress response.
A comprehensive meta-analysis examining stress reduction interventions in periodontal disease management found that patients combining conventional treatment with stress-management techniques achieved superior clinical outcomes, including greater probing depth reduction and enhanced attachment level gain. These findings suggest that mindfulness should be positioned as an integral component of comprehensive periodontal management rather than an optional adjunct.
Evidence also supports specific mindfulness applications for oral-related anxiety. Patients scheduled for periodontal procedures who completed brief mindfulness interventions reported significantly lower anxiety levels, reduced pain perception during treatment, and improved treatment satisfaction. This psychological benefit translates to enhanced treatment compliance and willingness to pursue necessary interventions that support long-term gingival health.

Practical Mindfulness Techniques for Oral Health
Implementing mindfulness practices requires minimal resources while delivering substantial benefits for gingival recession management. Body scan meditation represents an accessible starting point, involving systematic attention to physical sensations throughout the body. This practice cultivates awareness of tension patterns, including jaw clenching and facial muscle tension that exacerbate periodontal stress. Daily 10-15 minute body scan sessions train the nervous system toward relaxation while identifying unconscious oral habits.
Breath awareness meditation provides another foundational practice. Focusing attention on natural breathing patterns activates the parasympathetic nervous system and reduces cortisol production. The technique involves sitting comfortably, closing the eyes, and observing breath without attempting to control it. When attention wanders—which inevitably occurs—practitioners gently redirect focus to breathing. Even five minutes of daily breath awareness produces measurable reductions in stress markers and promotes oral tissue healing.
Mindful brushing and flossing transforms routine oral hygiene into therapeutic practice. Rather than mechanically rushing through dental care, patients bring full sensory awareness to tooth brushing—noticing the brush texture, water temperature, mint flavor, and gum sensations. This mindful approach enhances plaque removal effectiveness while strengthening the psychological connection between self-care behaviors and health outcomes. Mindful oral hygiene also prevents the aggressive brushing patterns that mechanically contribute to gingival recession.
Progressive muscle relaxation specifically targets the jaw and facial muscles implicated in stress-related bruxism and clenching. The technique involves systematically tensing and releasing muscle groups, with particular emphasis on the masseter, temporalis, and neck muscles. Regular practice reduces baseline muscle tension while training awareness of tension onset, enabling real-time intervention when clenching patterns emerge.
Loving-kindness meditation cultivates positive emotional states and self-compassion, addressing the psychological distress associated with visible gingival recession. This practice involves silently repeating phrases of goodwill toward oneself and others, gradually expanding the circle of compassion. Research demonstrates that loving-kindness meditation reduces inflammatory markers while enhancing immune function, creating dual benefits for periodontal healing.
Integrating Mindfulness with Professional Dental Care
Optimal management of gingival recession requires seamless integration between professional dental interventions and patient-directed mindfulness practice. Patients should maintain transparent communication with their dental providers regarding stress levels, anxiety, and psychological factors influencing their oral health. Dentists trained in psychosomatic medicine can incorporate mindfulness recommendations into comprehensive treatment plans, positioning stress reduction as a clinical priority equivalent to mechanical plaque removal.
The advancement of evidence-based medicine increasingly emphasizes interprofessional collaboration in managing complex conditions like periodontal disease. Dental professionals may collaborate with mental health specialists, primary care physicians, or wellness coaches to develop integrated care plans addressing both clinical and psychological dimensions. This comprehensive approach acknowledges that gingival recession supportive therapy extends beyond the dental operatory into the patient’s daily life and emotional landscape.
Patients should expect their dental team to provide guidance on oral hygiene techniques that minimize mechanical trauma while maximizing plaque removal. Soft-bristled toothbrushes, gentle technique instruction, and electric toothbrush recommendations reduce iatrogenic recession risk. Simultaneously, mindfulness training helps patients internalize these recommendations through body awareness rather than relying solely on external instruction.
Professional periodontal treatment options—including scaling and root planing, antimicrobial therapies, and in some cases surgical interventions—remain essential components of gingival recession management. Mindfulness practice enhances treatment tolerance, improves post-operative healing, and supports the behavioral changes necessary for long-term disease control. Patients who approach treatment with mindful acceptance rather than anxiety and resistance experience superior clinical outcomes and greater satisfaction with care.
Lifestyle Modifications to Support Gum Health
Beyond formal mindfulness practice, numerous lifestyle modifications synergistically support gingival health and stress reduction. Regular physical exercise reduces cortisol levels, enhances immune function, and improves mood through endogenous opioid release. Aerobic activity, strength training, and yoga all demonstrate benefits for periodontal disease markers. Yoga particularly combines physical movement with mindfulness principles, offering integrated mind-body benefits specifically relevant to oral health.
Dietary modifications significantly impact periodontal disease progression. Consuming whole foods rich in antioxidants, omega-3 fatty acids, and polyphenols reduces systemic inflammation and supports gum tissue healing. Conversely, processed foods, excessive sugar, and refined carbohydrates promote dysbiotic oral microbiota and systemic inflammation. A nutrient-dense diet represents both a stress-reduction tool and a direct intervention for periodontal disease.
Sleep quality profoundly influences immune function and stress hormone regulation. Patients with gingival recession should prioritize consistent sleep schedules, optimal sleep environment conditions, and pre-sleep mindfulness practices. Poor sleep perpetuates the inflammatory cascade driving periodontal disease and impairs tissue healing capacity. Addressing sleep disturbances through behavioral interventions and mindfulness represents a critical yet often overlooked component of comprehensive gum disease management.
Social connection and community engagement reduce isolation, enhance emotional resilience, and buffer against chronic stress. Participating in group mindfulness classes, support communities, or wellness programs provides both direct stress reduction benefits and the psychological comfort of shared experience. Research consistently demonstrates that socially connected individuals exhibit superior periodontal health outcomes compared to isolated counterparts.
Limiting caffeine and alcohol consumption reduces physiological arousal and supports sleep quality. Smoking cessation remains perhaps the most critical lifestyle modification, as tobacco use directly impairs periodontal healing and dramatically accelerates gingival recession progression. Mindfulness-based smoking cessation programs demonstrate superior efficacy compared to conventional approaches, suggesting that stress reduction represents a key mechanism through which individuals successfully quit.
Professionals working in occupational therapy and wellness fields recognize that sustainable lifestyle change requires addressing psychological barriers and building intrinsic motivation. Mindfulness cultivates this internal motivation by deepening awareness of how lifestyle choices impact physical sensation and well-being, creating powerful incentives for continued positive behavior modification.
FAQ
Can mindfulness alone cure gingival recession?
No, mindfulness cannot reverse established gingival recession independently. However, mindfulness serves as essential supportive therapy that complements professional dental treatment by reducing stress-driven inflammatory processes, improving treatment compliance, and supporting healing. Severe recession typically requires professional interventions including scaling, root planing, or surgical grafting, with mindfulness enhancing outcomes of these treatments.
How long does mindfulness practice take to show periodontal benefits?
Research indicates that measurable reductions in inflammatory markers occur within 6-8 weeks of consistent mindfulness practice, with optimal benefits emerging after 12+ weeks. However, subjective stress reduction and improved oral awareness develop within days. Patients should maintain realistic expectations while committing to long-term practice as part of comprehensive gingival recession supportive therapy.
Is mindfulness appropriate for patients with severe anxiety about dental treatment?
Yes, mindfulness proves particularly beneficial for dental anxiety. Pre-treatment mindfulness practice reduces anxiety levels, pain perception, and treatment avoidance. Dentists can teach brief mindfulness techniques performed before and during procedures. For severe dental phobia, mindfulness may be combined with professional mental health support and graduated exposure therapy.
What type of mindfulness practice works best for oral health?
Evidence supports multiple approaches, with optimal results emerging from combined practice including meditation (10-15 minutes daily), mindful brushing/flossing, body awareness, and stress-reduction activities like yoga or tai chi. Individual preferences determine which practices prove sustainable, so experimentation to identify personally resonant approaches maximizes adherence and benefit.
Should I discontinue professional dental treatment if I practice mindfulness?
Absolutely not. Mindfulness represents supportive therapy complementing, never replacing, professional dental care. Patients must maintain regular dental visits, follow professional treatment recommendations, and practice rigorous oral hygiene. Mindfulness enhances these essential interventions rather than substituting for them.
Can stress reduction reverse gingival recession?
Stress reduction cannot reverse existing tissue loss but prevents further recession progression by reducing inflammatory drivers of periodontal disease. Some research suggests that reducing chronic stress may support modest tissue regeneration in early-stage recession, though professional interventions remain necessary for significant tissue recovery.