
Is Hyperbaric Oxygen Therapy Effective? Expert Insights
Hyperbaric oxygen therapy (HBOT) has emerged as a compelling treatment modality that continues to generate both enthusiasm and debate within the medical community. This specialized therapy involves breathing pure oxygen in a pressurized chamber, allowing your lungs to gather more oxygen than would be possible at normal atmospheric pressure. The increased oxygen availability then circulates throughout your bloodstream, potentially enhancing healing and reducing inflammation in affected tissues.
For residents and patients in hyperbaric oxygen therapy Palm Coast and surrounding Florida communities, understanding the effectiveness of this treatment is crucial for making informed healthcare decisions. Whether you’re considering HBOT for wound healing, diving injuries, or other medical conditions, this comprehensive guide examines the scientific evidence, clinical applications, and expert perspectives on this increasingly popular therapy.
How Hyperbaric Oxygen Therapy Works
Hyperbaric oxygen therapy operates on fundamental principles of physics and physiology. When you enter a hyperbaric chamber pressurized to 2.4 to 3.0 atmospheres absolute (ATA), the increased pressure allows your lungs to absorb significantly more oxygen than at sea level. According to peer-reviewed research on hyperbaric medicine, oxygen dissolves directly into your blood plasma at these pressures, bypassing normal hemoglobin saturation limits.
This mechanism creates several therapeutic cascades: enhanced angiogenesis (new blood vessel formation), improved white blood cell function for fighting infection, reduced edema through osmotic effects, and increased fibroblast activity that accelerates collagen synthesis. The therapy typically involves sessions lasting 90 to 120 minutes, conducted in either monoplace chambers (single-patient) or multiplace chambers (accommodating multiple patients and medical personnel). Understanding how long the effects of hyperbaric oxygen therapy last helps patients establish realistic treatment expectations and recovery timelines.
The physiological response isn’t instantaneous—most protocols require multiple sessions, typically ranging from 20 to 40 treatments depending on the condition being treated. Each session allows your body to mobilize repair mechanisms at the cellular level, gradually improving tissue oxygenation and promoting healing in previously compromised areas.

FDA-Approved Conditions and Clinical Evidence
The Food and Drug Administration has officially approved hyperbaric oxygen therapy for 14 specific indications, providing a scientifically validated foundation for HBOT’s effectiveness. These approved conditions include air or gas embolism, carbon monoxide poisoning, decompression sickness (the bends), diabetic wounds, exceptional blood loss anemia, gangrene, intracranial abscess, necrotizing soft tissue infections, osteomyelitis, radiation tissue damage, skin grafts and flaps, and thermal burns.
For each of these conditions, clinical trials and observational studies have demonstrated measurable benefits. Comprehensive reviews in medical literature show that HBOT significantly improves healing rates in diabetic foot ulcers, with some studies reporting complete healing in 40-60% of previously non-responsive wounds. The therapy’s effectiveness for carbon monoxide poisoning is particularly robust, with evidence showing it reduces cognitive sequelae when administered within specific timeframes after exposure.
Expert consensus from organizations like the Undersea and Hyperbaric Medical Society (UHMS) confirms that HBOT delivers measurable clinical outcomes when properly indicated and administered. However, effectiveness varies considerably depending on patient selection, underlying health conditions, treatment protocol adherence, and the specific pathology being addressed.
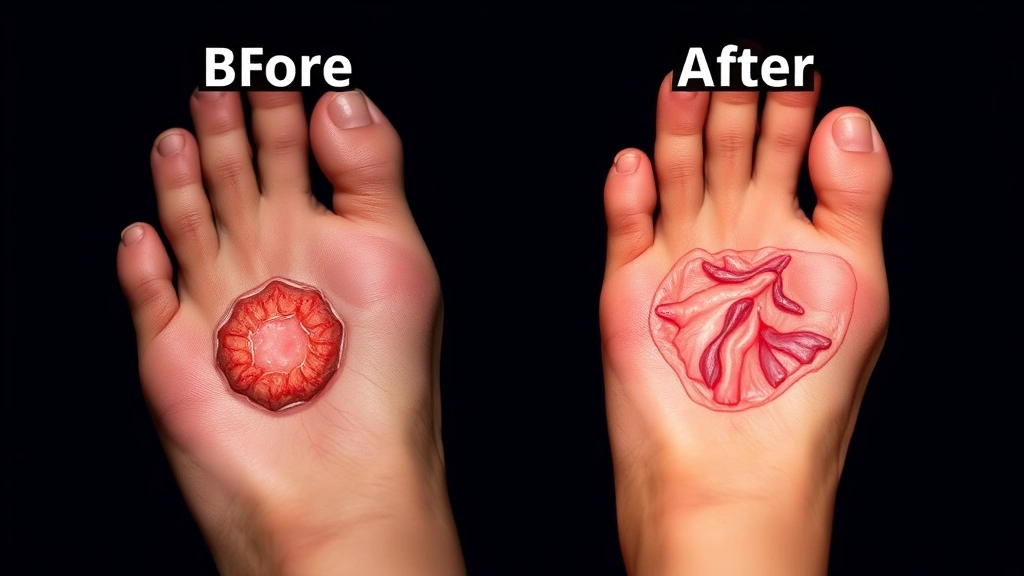
Effectiveness for Chronic Wounds and Diabetic Ulcers
Chronic wounds represent one of the most compelling applications for hyperbaric oxygen therapy, particularly diabetic ulcers that resist conventional treatment. Approximately 15-25% of diabetic patients develop foot ulcers during their lifetime, and roughly 5-10% of these progress to amputation. HBOT offers a potentially limb-saving intervention for this vulnerable population.
The mechanism proves particularly effective for diabetic wounds because the therapy addresses the fundamental pathophysiology: impaired angiogenesis, reduced immune function, and chronic hypoxia. By restoring adequate tissue oxygen levels, HBOT enables the body’s natural healing cascade. Clinical evidence demonstrates that diabetic foot ulcers treated with HBOT show significantly improved healing rates compared to standard wound care alone.
A pivotal clinical trial published in medical literature showed that adding HBOT to standard care increased the likelihood of complete ulcer healing by approximately 50% within the study period. For patients considering this therapy in Palm Coast, understanding these evidence-based outcomes helps contextualize the treatment within a comprehensive wound care strategy. Exploring additional therapy resources and information through reliable medical sources enhances your decision-making process.
However, effectiveness depends on several factors: ulcer duration (newer wounds respond better), adequate blood supply to the affected limb, appropriate wound care between sessions, and patient compliance with the full treatment protocol. Patients with severe peripheral vascular disease may not respond adequately to HBOT alone.
HBOT for Sports Injuries and Recovery
Athletes and active individuals increasingly explore hyperbaric oxygen therapy for accelerating recovery from injuries and enhancing performance. While HBOT isn’t FDA-approved specifically for sports injuries, off-label use has generated considerable interest and anecdotal support within athletic communities.
The theoretical basis appears sound: enhanced oxygen delivery should theoretically reduce inflammation, accelerate tissue repair, and potentially minimize recovery time. Some professional athletes and sports medicine practitioners report subjective improvements in healing timelines for muscle strains, ligament sprains, and stress fractures. However, the scientific evidence supporting these claims remains more limited compared to FDA-approved indications.
Research examining HBOT for sports-related injuries shows mixed results. While some studies suggest modest benefits for certain acute injuries, the evidence base doesn’t yet support routine HBOT as standard sports medicine practice. Understanding how long physical therapy typically takes provides context for comparing recovery timelines across different therapeutic modalities.
For Palm Coast residents interested in HBOT for athletic recovery, consulting with both your sports medicine physician and hyperbaric medicine specialist helps establish realistic expectations. The therapy may offer complementary benefits when integrated into comprehensive rehabilitation programs, though it shouldn’t replace evidence-based physical therapy and other proven recovery strategies.
Off-Label Uses and Emerging Research
Beyond FDA-approved indications, researchers investigate hyperbaric oxygen therapy for numerous conditions including autism spectrum disorder, cerebral palsy, fibromyalgia, multiple sclerosis, Parkinson’s disease, and post-stroke recovery. These investigations reflect genuine scientific curiosity about HBOT’s potential neuroprotective and neuroplastic effects.
The neurological applications prove particularly intriguing because chronic hypoxia contributes to neurodegeneration in various conditions. Theoretically, enhancing cerebral oxygen delivery might slow disease progression or improve functional outcomes. However, current evidence for most off-label neurological applications remains preliminary, typically limited to small studies, case reports, or animal research.
Several clinical trials are currently underway examining HBOT’s efficacy for conditions like long COVID, traumatic brain injury, and radiation-induced tissue damage. The National Institutes of Health Clinical Trials database tracks these investigations, allowing interested patients to follow emerging evidence as it develops.
It’s crucial to distinguish between promising preliminary research and proven clinical effectiveness. Patients considering HBOT for off-label indications should understand that while scientific rationale may exist, robust clinical evidence supporting these applications hasn’t yet been established. Evaluating whether therapy actually works requires examining the totality of scientific evidence rather than relying solely on theoretical mechanisms or anecdotal reports.
Safety Profile and Side Effects
Hyperbaric oxygen therapy demonstrates a relatively favorable safety profile when administered by qualified practitioners in appropriate facilities. The most common side effects are mild and temporary, including ear barotrauma (pressure-related ear discomfort), sinus barotrauma, and claustrophobic anxiety in enclosed chambers.
More serious but rare complications include oxygen toxicity (manifesting as visual changes, tinnitus, nausea, or seizures), barotrauma to the lungs, and temporary myopia (nearsightedness). Decompression sickness theoretically could occur with improper decompression protocols, though modern equipment and trained operators minimize this risk substantially.
Patients with certain conditions require medical clearance before HBOT: uncontrolled fever, recent chemotherapy, claustrophobia, or history of thoracic surgery. Additionally, diabetic patients taking certain medications must monitor blood glucose carefully, as HBOT can temporarily affect glucose metabolism. Considering physical therapy costs alongside HBOT expenses helps establish realistic healthcare budgets.
The Undersea and Hyperbaric Medical Society maintains rigorous safety standards and certification requirements for facilities and practitioners. Choosing an accredited facility with board-certified hyperbaric medicine physicians significantly reduces adverse event risks.
Finding HBOT Services in Palm Coast
Palm Coast residents seeking hyperbaric oxygen therapy should prioritize facilities meeting established safety and quality standards. Look for centers staffed by physicians certified in hyperbaric and diving medicine, accreditation from recognized hyperbaric medicine organizations, and clear protocols for patient evaluation and monitoring.
When evaluating potential providers, ask about their experience treating your specific condition, the number of sessions they recommend, expected outcomes based on similar cases, and what comprehensive wound care or adjunctive therapies they provide alongside HBOT. Reputable facilities conduct thorough initial assessments, establish clear treatment plans with defined endpoints, and maintain detailed outcome tracking.
Insurance coverage varies considerably depending on your plan and the condition being treated. FDA-approved indications typically receive better coverage than off-label applications. Contact your insurance provider directly and request information about their HBOT coverage policies, authorization requirements, and cost-sharing obligations.
Setting realistic therapy goals with your healthcare team ensures HBOT integrates appropriately within your broader treatment strategy. For chronic conditions, HBOT works most effectively as part of comprehensive care plans rather than as isolated therapy.
Frequently Asked Questions
Is hyperbaric oxygen therapy covered by insurance?
Coverage depends on your specific insurance plan and whether the condition falls within FDA-approved indications. Diabetic ulcers, chronic wounds, and other approved conditions typically receive coverage when medically necessary and prescribed by qualified physicians. Off-label applications rarely receive insurance reimbursement. Contact your insurance provider for definitive coverage information.
How many HBOT sessions do most patients require?
Treatment protocols vary based on the condition and individual response. Typical courses range from 20 to 40 sessions, though some conditions may require more or fewer treatments. Your hyperbaric medicine physician establishes a specific protocol after thorough evaluation.
Can hyperbaric oxygen therapy cure my condition permanently?
HBOT facilitates healing and improves tissue oxygenation, but it’s not universally curative. For some conditions like carbon monoxide poisoning or diabetic ulcers, HBOT can provide substantial healing. For chronic conditions, benefits may be temporary and require maintenance therapy. Realistic expectations should be established with your medical team.
What’s the difference between monoplace and multiplace chambers?
Monoplace chambers accommodate a single patient and operate on slightly different pressure principles. Multiplace chambers hold multiple patients and medical personnel, allowing direct physician presence during treatment. Both are effective when properly maintained and operated by trained staff.
Are there any long-term effects from repeated HBOT sessions?
When administered appropriately by qualified practitioners, repeated HBOT sessions demonstrate excellent long-term safety profiles. The most common long-term effect is temporary myopia, which typically resolves after treatment completion. Serious long-term complications are exceptionally rare.
How quickly will I see results from hyperbaric oxygen therapy?
Some patients notice improvements within the first few sessions, while others require weeks of treatment before measurable progress appears. Chronic wounds typically show gradual improvement over multiple sessions. Individual response varies considerably based on age, overall health, and the specific condition being treated.



