Is Hyperbaric Oxygen Therapy Effective? Expert Insights and Evidence-Based Analysis
Hyperbaric oxygen therapy (HBOT) has gained considerable attention in recent years as a potential treatment for various medical conditions, from wound healing to neurological disorders. If you’re exploring treatment options in Mount Vernon, WA, or anywhere else, understanding the scientific evidence behind HBOT is essential for making informed healthcare decisions. This comprehensive guide examines the current research, clinical applications, and expert perspectives on hyperbaric oxygen therapy’s effectiveness.
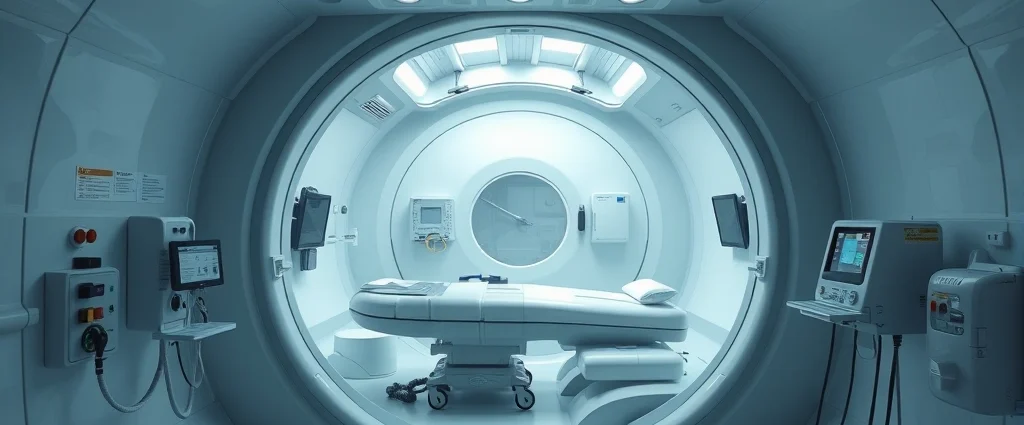
Hyperbaric oxygen therapy involves breathing pure oxygen in a pressurized chamber, typically at 2-3 times normal atmospheric pressure. The increased pressure allows your lungs to gather significantly more oxygen than would be possible at normal air pressure, which then circulates throughout your bloodstream. Proponents claim this enhanced oxygen delivery promotes healing and reduces inflammation, but the scientific community remains divided on its broader applications beyond established medical uses.
How Hyperbaric Oxygen Therapy Works
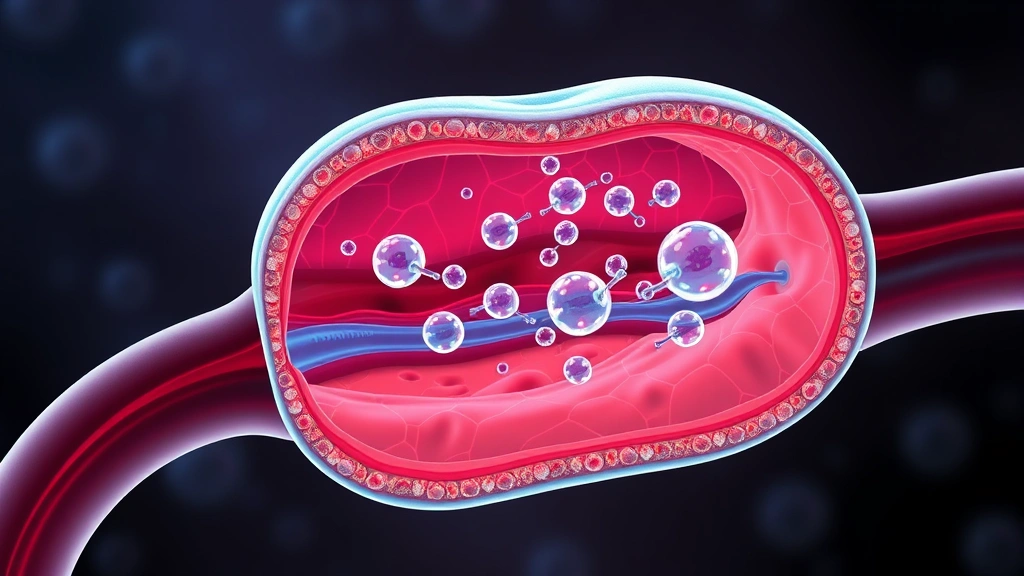
The physiological mechanisms underlying hyperbaric oxygen therapy are straightforward but powerful. When you enter a hyperbaric chamber pressurized to 2.8 atmospheres absolute (ATA), the partial pressure of oxygen in your blood increases dramatically. Under normal conditions, oxygen travels through your bloodstream attached to hemoglobin molecules. However, HBOT forces additional oxygen into your plasma—the liquid component of blood—allowing it to reach areas with compromised blood flow more effectively.
This increased oxygen availability triggers several biological responses. Enhanced oxygen delivery stimulates angiogenesis, the formation of new blood vessels, which improves circulation to damaged tissues. Additionally, the therapy promotes collagen synthesis, essential for wound healing and tissue repair. Oxygen also possesses antimicrobial properties, helping combat infections in wounds and supporting immune function. Furthermore, HBOT reduces tissue edema (swelling) by decreasing inflammatory markers and promoting fluid reabsorption.
The therapy typically involves 40-60 minute sessions in a monoplace chamber (accommodating one person) or multiplace chamber (accommodating multiple patients). Treatment protocols vary depending on the condition being treated, with most established applications requiring 20-40 sessions over several weeks. The cumulative effect of multiple sessions allows tissues to gradually improve their oxygen-dependent healing processes.
FDA-Approved Medical Applications
The Food and Drug Administration has officially approved hyperbaric oxygen therapy for 14 specific medical conditions. Understanding these approved uses helps distinguish between evidence-based applications and experimental treatments. The most well-established applications include:
- Diabetic foot ulcers – HBOT significantly improves healing rates in patients with chronic diabetic wounds, particularly those unresponsive to conventional treatment
- Chronic wounds and non-healing wounds – Including venous stasis ulcers and pressure wounds resistant to standard care
- Carbon monoxide poisoning – HBOT rapidly eliminates carbon monoxide from tissues and prevents delayed neurological syndrome
- Gas embolism – Decompression sickness from diving accidents responds dramatically to HBOT
- Osteomyelitis – Chronic bone infections benefit from improved oxygen delivery to infected bone tissue
- Radiation tissue damage – Both acute and chronic radiation injuries show improvement with HBOT
- Necrotizing soft tissue infections – HBOT supports immune function in treating aggressive bacterial infections
These FDA-approved applications have substantial clinical evidence supporting their use. If you’re considering therapy resources and treatment options, it’s important to verify that your specific condition falls within these established categories. Research from the Undersea and Hyperbaric Medical Society provides comprehensive guidelines on approved indications and treatment protocols.
Research on Off-Label Uses
Beyond FDA-approved applications, researchers have investigated hyperbaric oxygen therapy for numerous conditions with varying degrees of success. Understanding the quality of evidence for these off-label uses is crucial for realistic expectations.
Autism Spectrum Disorder: Several small studies suggested HBOT might improve autism symptoms, but larger, well-controlled trials have failed to demonstrate significant benefits. A 2015 review in PLOS Medicine found insufficient evidence to recommend HBOT as an autism treatment, despite enthusiastic promotion by some practitioners.
Traumatic Brain Injury and Concussion: While oxygen delivery to brain tissue is theoretically beneficial, clinical trials have shown mixed results. Some studies indicate modest improvements in cognitive function, but the evidence isn’t strong enough for routine clinical recommendation. Researchers continue investigating optimal protocols and patient selection criteria.
Post-Lyme Disease Syndrome: Limited evidence suggests HBOT might help some chronic Lyme disease patients, but rigorous studies are lacking. The condition’s complex nature makes it difficult to isolate HBOT’s specific effects from other treatments.
Fibromyalgia: A small Israeli study reported improvements in fibromyalgia symptoms with HBOT, but replication studies have produced inconsistent results. Patient selection and specific treatment protocols may significantly influence outcomes.
Hair Loss: Some clinics promote HBOT for alopecia, but clinical evidence is minimal. While improved blood flow theoretically benefits hair follicles, controlled studies haven’t demonstrated clinically significant hair regrowth.
When evaluating off-label applications, consult research from peer-reviewed journals rather than promotional materials. The distinction between whether therapy works for your specific condition requires critical assessment of study design, sample sizes, and peer review status.

Safety Considerations and Side Effects
Hyperbaric oxygen therapy is generally considered safe when administered by qualified professionals following established protocols. However, understanding potential risks helps you make informed decisions about treatment.
Common Side Effects: Most patients experience mild, temporary effects including ear and sinus pressure (similar to airplane cabin pressure changes), mild claustrophobia in monoplace chambers, and temporary myopia (nearsightedness) that typically resolves after therapy completion. These effects rarely necessitate treatment discontinuation.
Oxygen Toxicity: Breathing pure oxygen under pressure carries a small risk of oxygen toxicity, which can cause seizures in rare cases (approximately 1-2 per 10,000 treatments). Proper training, adherence to depth and time limits, and medical supervision minimize this risk significantly. Patients taking certain medications or with specific medical conditions face elevated risk and require careful screening.
Barotrauma: Pressure-related injuries to the ears or sinuses can occur if patients can’t equalize pressure during compression and decompression. Proper equalization techniques and gradual pressure changes prevent this complication in nearly all cases.
Contraindications: Certain conditions make HBOT inappropriate, including uncontrolled fever, history of thoracic surgery, and active chemotherapy with specific agents. Patients with claustrophobia or uncontrolled seizure disorders require careful evaluation before treatment.
When exploring treatment options, understanding therapy costs and safety profiles helps you weigh benefits against risks comprehensively. Always ensure treatment facilities maintain proper certification and staff credentials.
Cost and Accessibility in Mount Vernon
Hyperbaric oxygen therapy represents a significant financial investment, with costs varying substantially based on location, facility type, and treatment protocol. In Mount Vernon, WA, and surrounding communities, understanding pricing and insurance coverage is essential for treatment planning.
Typical Cost Structure: Individual HBOT sessions generally range from $200 to $400 per treatment in most U.S. markets. Complete treatment courses for FDA-approved conditions typically involve 20-40 sessions, resulting in total costs between $4,000 and $16,000. Some facilities offer package pricing that reduces per-session costs for multiple treatments.
Insurance Coverage: Medicare and most private insurance plans cover HBOT for FDA-approved indications when prescribed by a physician. Coverage for off-label uses is significantly less likely and varies by insurance provider. Verify coverage with your insurance company before committing to treatment, as out-of-pocket costs for uncovered treatments can be substantial.
Facility Options: Mount Vernon, WA residents have access to several healthcare facilities offering HBOT. Hospital-based programs typically provide the most comprehensive medical oversight and integrated care, while private clinics may offer more flexible scheduling. Research facility accreditation through the Undersea and Hyperbaric Medical Society to ensure proper standards and qualified personnel.
Comparing HBOT costs with alternative treatment approaches helps determine the most cost-effective path forward. Understanding how long physical therapy takes and its associated costs provides valuable context for evaluating multiple treatment options.
Comparing HBOT to Alternative Therapies
Evaluating hyperbaric oxygen therapy requires considering how it compares to other established treatments for similar conditions. Different therapies excel in different contexts.
HBOT vs. Conventional Wound Care: For diabetic foot ulcers and chronic wounds, HBOT significantly improves healing when combined with standard wound care (debridement, infection control, pressure relief). However, HBOT alone without proper wound management provides minimal benefit. The combination approach yields superior outcomes compared to either treatment independently.
HBOT vs. Surgical Interventions: For some conditions like chronic osteomyelitis, HBOT may reduce the need for extensive surgical debridement or amputation. However, it typically complements rather than replaces surgical treatment. Discussing the role of HBOT within your overall surgical plan with your surgeon ensures optimal outcomes.
HBOT vs. Red Light Therapy: Red light therapy for back pain and other conditions works through different mechanisms than HBOT. Red light therapy stimulates cellular energy production and reduces inflammation through photobiomodulation, while HBOT delivers oxygen directly to tissues. These therapies target different biological pathways and may complement each other in some treatment protocols.
HBOT vs. Pharmaceutical Interventions: For conditions like diabetic neuropathy or chronic pain, HBOT offers a non-pharmaceutical approach that avoids medication side effects. However, pharmaceutical treatments may provide faster symptom relief while HBOT addresses underlying tissue healing. Combining approaches often yields better results than monotherapy.
Evidence Quality Across Therapies: When comparing treatment options, examine the strength of clinical evidence supporting each approach. FDA-approved HBOT indications have substantial evidence, while many alternative therapies lack similarly rigorous research. This doesn’t necessarily mean alternatives are ineffective, but rather that their efficacy requires more investigation.
The most effective treatment plan often integrates multiple modalities tailored to your specific condition. Consulting with healthcare providers experienced in your particular condition helps identify the optimal combination of therapies, whether that includes HBOT or other interventions. Understanding how therapy works across different domains helps you evaluate treatment recommendations critically.
Frequently Asked Questions
How many HBOT sessions do most patients need?
The number of sessions varies significantly depending on the condition being treated. FDA-approved indications typically require 20-40 sessions, with each session lasting 90-120 minutes including compression and decompression time. Your physician will recommend a specific protocol based on your condition, severity, and response to initial treatments. Some patients show improvement within 10-15 sessions, while others require the full recommended course.
Is hyperbaric oxygen therapy painful?
HBOT itself is painless, but patients may experience pressure sensations in their ears and sinuses similar to airplane cabin pressure changes. Learning proper equalization techniques (Valsalva maneuver) before treatment prevents discomfort. Some patients experience mild claustrophobia in monoplace chambers, though multiplace chambers accommodate this concern better. Most discomfort is minimal and temporary.
Can HBOT cure my condition permanently?
HBOT promotes healing and tissue repair but doesn’t cure underlying diseases. For example, while HBOT helps diabetic foot ulcers heal, it doesn’t cure diabetes itself. The therapy works best for conditions where improved oxygen delivery directly facilitates healing. For chronic conditions, you may need ongoing management even after completing HBOT.
Are there any long-term effects from HBOT?
When administered properly by qualified professionals, HBOT has an excellent long-term safety profile. Most patients experience no lasting negative effects. Some patients report temporary myopia (nearsightedness) that typically resolves within weeks after treatment completion. The long-term benefits for approved indications generally outweigh minimal risks when proper protocols are followed.
How does HBOT compare to other oxygen therapies?
HBOT differs fundamentally from supplemental oxygen therapy or hypoxic training. HBOT uses pressurized chambers to force oxygen into tissues at much higher concentrations than other oxygen therapies achieve. While supplemental oxygen helps patients with respiratory conditions maintain adequate oxygen levels, HBOT specifically targets tissue repair through supraphysiologic oxygen delivery.
Can I use HBOT if I’m claustrophobic?
Patients with claustrophobia have options, though treatment requires careful planning. Multiplace chambers, which accommodate multiple patients and a technician, feel less claustrophobic than monoplace chambers. Some facilities offer gradual acclimation sessions to help claustrophobic patients adapt. Discuss your concerns with your treatment facility—they may recommend anxiety management techniques or alternative facilities better suited to your needs.
Does insurance cover HBOT in Mount Vernon, WA?
Insurance coverage for HBOT in Mount Vernon depends on your specific plan and whether your condition falls within FDA-approved indications. Medicare covers HBOT for approved conditions with physician prescription. Most private insurance plans provide similar coverage, but verification with your insurance provider is essential before starting treatment. Off-label uses typically require out-of-pocket payment.