
How Long Does HBOT Last? Expert Insights on Hyperbaric Oxygen Therapy Duration
Hyperbaric oxygen therapy (HBOT) has emerged as a compelling treatment modality for various medical conditions, from chronic wounds to decompression sickness. However, one of the most pressing questions patients ask is: how long do the effects of hyperbaric oxygen therapy actually last? The answer is nuanced and depends on multiple factors including the condition being treated, individual physiology, and treatment protocols.
Understanding the duration and longevity of HBOT benefits requires examining both the immediate physiological responses and long-term therapeutic outcomes. This comprehensive guide explores what research reveals about HBOT effectiveness timelines and provides practical insights for patients considering this treatment option.
Understanding Hyperbaric Oxygen Therapy Basics
Hyperbaric oxygen therapy involves breathing pure oxygen in a pressurized chamber, typically at pressures greater than atmospheric pressure at sea level. The increased pressure allows oxygen to dissolve more effectively into the bloodstream and body tissues, promoting healing and reducing inflammation. Standard HBOT sessions last approximately 90 to 120 minutes, with patients typically undergoing multiple sessions over weeks or months depending on their condition.
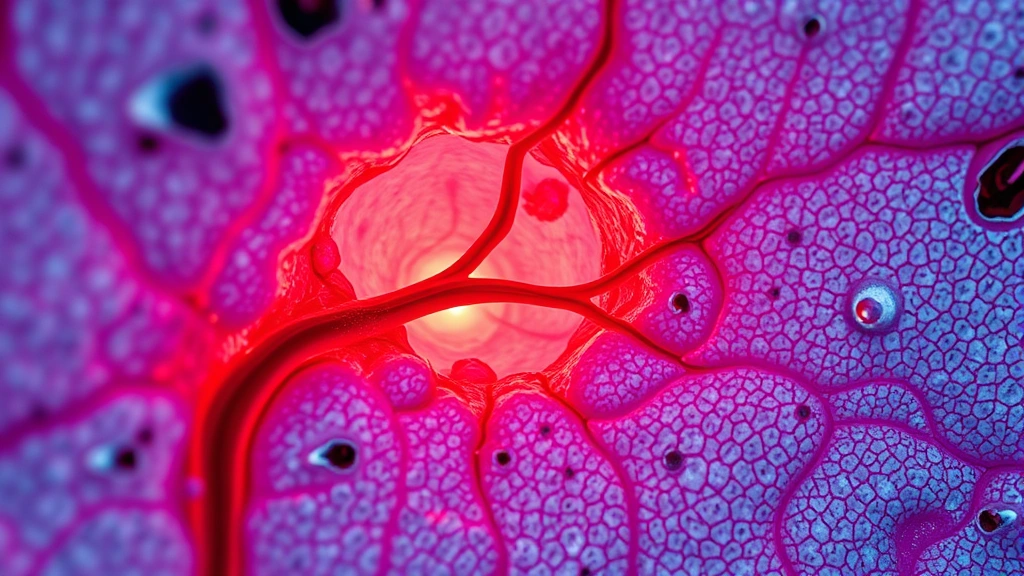
The therapy works through several mechanisms: increasing oxygen partial pressure in tissues, promoting neovascularization (new blood vessel formation), enhancing white blood cell function, and reducing edema. These physiological changes create a cascade of healing responses that extend beyond the treatment chamber itself. Understanding these mechanisms helps explain why HBOT effects persist for varying durations after individual sessions conclude.
When considering physical therapy cost comparisons, HBOT represents a significant investment. However, the potential for lasting therapeutic benefits makes it attractive for patients with conditions resistant to conventional treatments. The cost-benefit analysis becomes clearer when understanding how long effects typically last.

Duration of HBOT Effects by Condition
The longevity of HBOT effects varies dramatically depending on the specific medical condition being treated. Chronic diabetic wounds, one of the most common HBOT applications, often show sustained benefits for months to years after completing a full treatment course. Patients frequently experience continued wound healing improvements for 6-12 months following their final session, with some experiencing benefits extending beyond this timeframe.
For acute conditions like carbon monoxide poisoning or decompression sickness, HBOT effects are typically more immediate and sustained. Patients often report symptom resolution that persists indefinitely once the acute crisis has been addressed. The underlying tissue damage has been repaired, and the physiological correction achieved through HBOT remains stable.
Radiation injury treatment presents another scenario where HBOT duration varies. Patients with radiation-induced tissue damage may experience progressive improvement for 12-24 months after completing treatment, as the enhanced blood flow and tissue regeneration continue supporting healing long after sessions end. Some conditions, like osteonecrosis, show remarkable durability in HBOT benefits, with many patients maintaining improvement for years.
Neurological conditions such as stroke-related deficits show more variable outcomes. Some patients report sustained cognitive and motor improvements, while others experience gradual return of symptoms over weeks or months. This variability underscores the importance of understanding individual response patterns.
Immediate vs Long-Term Benefits
HBOT produces both immediate and delayed therapeutic effects. Immediately following sessions, patients often report increased energy, mental clarity, and reduced pain—benefits that typically persist for several hours to days. These immediate effects result from acute oxygen saturation and reduced inflammation.
Long-term benefits emerge over the course of treatment as cumulative sessions produce structural tissue changes. New blood vessel formation, improved collagen deposition, and enhanced cellular regeneration create benefits that accumulate throughout the treatment course. These long-term changes often persist well beyond the final session because the underlying tissue architecture has been permanently altered.
Research published in peer-reviewed medical journals demonstrates that the most durable benefits come from these structural changes rather than acute oxygen saturation effects. This explains why patients who complete full treatment courses typically experience longer-lasting benefits than those who discontinue treatment prematurely.
The distinction between immediate and long-term effects has important implications for treatment planning. While some patients seek HBOT primarily for immediate symptom relief, optimal outcomes typically require committing to complete treatment protocols designed to achieve lasting structural tissue modifications.
Factors Affecting HBOT Duration
Multiple variables influence how long HBOT effects persist. Patient age represents a significant factor—younger patients typically show more robust and durable healing responses than older individuals, whose tissue regeneration capacity naturally declines with age. However, even elderly patients frequently experience substantial lasting benefits.
The severity and chronicity of the underlying condition profoundly impacts effect duration. Acute conditions often respond more dramatically and durably than chronic problems that have persisted for years. A patient with a diabetic foot ulcer of recent onset typically achieves longer-lasting benefits than someone with a chronic non-healing wound present for multiple years.
Individual metabolic factors, including diabetes control, nutritional status, and cardiovascular health, significantly influence HBOT efficacy and durability. Patients with well-controlled metabolic conditions generally experience more sustained benefits. Conversely, patients with poorly controlled diabetes or significant nutritional deficiencies may experience more modest and shorter-lasting improvements.
Treatment protocol adherence substantially affects outcomes. Patients completing their prescribed full course of HBOT typically experience more durable benefits than those discontinuing treatment early. The cumulative effect of multiple sessions appears essential for achieving lasting tissue modifications.
Smoking status deserves particular mention as a critical determinant. Smoking significantly impairs oxygen utilization and tissue healing, reducing both the immediate effectiveness of HBOT and the durability of benefits. Patients who quit smoking before or during HBOT typically achieve substantially better long-term outcomes.
Concurrent medical conditions, medications, and lifestyle factors all contribute to determining how long therapeutic benefits persist. A holistic approach addressing these variables typically produces the most durable results.
Maintenance and Follow-Up Treatments
Some patients benefit from periodic maintenance HBOT sessions following their initial treatment course. These maintenance sessions can help sustain improvements, particularly for chronic conditions prone to recurrence. The frequency and necessity of maintenance therapy varies considerably depending on the specific condition and individual response patterns.
For chronic wounds, some physicians recommend occasional maintenance sessions to prevent relapse, particularly if the underlying risk factors (such as diabetes) remain active. These maintenance protocols typically involve far fewer sessions than initial treatment courses—often ranging from monthly to quarterly visits rather than daily sessions over weeks.
The decision to pursue maintenance therapy should involve careful discussion between patients and their HBOT physicians. Factors to consider include treatment effectiveness, condition severity, recurrence risk, and cost-benefit analysis. When considering therapy resources and articles on ongoing treatment, patients often discover that maintenance approaches offer a balanced strategy between achieving lasting benefits and managing long-term healthcare costs.
Some conditions naturally resolve and require no follow-up therapy whatsoever. Acute decompression sickness, once successfully treated, typically requires no maintenance protocol. The distinction between conditions requiring ongoing support versus those achieving permanent resolution represents an important treatment consideration.
Clinical Evidence and Research Findings
Substantial clinical evidence supports HBOT’s effectiveness for numerous conditions, though research also reveals important nuances about effect duration. A comprehensive review published in the Cochrane Database of Systematic Reviews examined HBOT efficacy across multiple conditions, documenting both the magnitude and duration of therapeutic benefits.
Studies examining diabetic foot ulcers demonstrate healing rates significantly higher with HBOT than conventional treatment alone. Importantly, follow-up assessments conducted 12 months post-treatment reveal sustained improvements in the majority of patients, with ulcer recurrence rates substantially lower in HBOT-treated groups compared to controls.
Research on radiation injury treatment from institutions including major cancer centers shows that HBOT effects often persist for years. Patients treated for radiation-induced soft tissue and bone injury frequently maintain improvement decades after completing therapy, suggesting that HBOT-induced tissue remodeling produces durable structural changes.
Neurological applications present more variable research findings. Studies examining HBOT for stroke recovery show promising short-term improvements in some patients, though long-term durability varies considerably. This variability has prompted ongoing research to identify which patient populations achieve the most sustained neurological benefits.
A study published in Undersea and Hyperbaric Medicine journal tracked HBOT patients over extended follow-up periods, documenting that approximately 70-80% of patients who completed full treatment courses maintained substantial clinical improvements at 12-month follow-up. This data provides reassuring evidence that HBOT effects often prove quite durable when treatment protocols are properly completed.
Comparing HBOT with Other Therapies
When evaluating HBOT, understanding how its effect duration compares with alternative treatments provides important context. Unlike some pharmaceutical interventions that require ongoing dosing to maintain benefits, HBOT often produces effects that persist long after treatment concludes. This represents a significant advantage for chronic conditions where long-term medication use might otherwise be necessary.
Compared with red light therapy for back pain and other modalities, HBOT typically produces more profound and durable effects, though individual responses vary. The mechanism of action differs substantially—HBOT works through enhanced oxygenation and tissue regeneration, while other therapies operate through different biological pathways.
For wound healing, HBOT demonstrates superior outcomes compared to standard dressing protocols alone, with benefits persisting substantially longer. The tissue remodeling induced by HBOT creates structural changes that conventional wound care cannot achieve, explaining the durability advantage.
Regarding cost-effectiveness, while HBOT requires substantial upfront investment, the long-lasting nature of benefits often provides superior value compared with ongoing treatments requiring continuous expenditure. Understanding these comparative advantages helps patients make informed treatment decisions aligned with their health goals and financial circumstances.
Maximizing HBOT Longevity: Practical Recommendations
Patients seeking to maximize the duration of HBOT benefits should prioritize several key strategies. First, completing the full prescribed treatment course substantially improves outcome durability. Discontinuing treatment prematurely significantly compromises long-term benefits, so committing to the complete protocol deserves emphasis.
Optimizing modifiable risk factors throughout and after treatment enhances HBOT efficacy. For diabetic patients, achieving and maintaining excellent glucose control amplifies HBOT benefits and extends their duration. Smoking cessation represents perhaps the single most impactful behavioral modification, as smoking directly impairs oxygen utilization and tissue healing.
Maintaining excellent nutrition and hydration supports the tissue regeneration processes that HBOT initiates. Patients should ensure adequate protein intake, micronutrient sufficiency, and consistent hydration throughout treatment and recovery periods. These nutritional factors significantly influence healing capacity and the durability of HBOT-induced improvements.
Appropriate wound care and infection prevention remain critical for patients undergoing HBOT for chronic wounds. While HBOT dramatically improves healing capacity, maintaining proper local wound management ensures that the therapy’s benefits translate into sustained clinical improvement.
Regular follow-up with HBOT physicians allows for monitoring of treatment response and discussion of maintenance protocols if appropriate. These clinical relationships provide opportunities to optimize long-term outcomes and address any emerging concerns about treatment durability.
Frequently Asked Questions
How long after HBOT will I feel better?
Many patients report feeling improved energy and reduced symptoms within the first few sessions, though dramatic improvements typically emerge over weeks of treatment. The timeline varies significantly depending on the condition being treated and individual healing capacity. Acute conditions often show rapid improvement, while chronic conditions typically require more extended treatment periods before substantial benefits manifest.
Do HBOT effects fade over time?
The durability of HBOT effects varies by condition. Many patients experience sustained benefits for months to years following treatment completion. Some conditions show permanent improvement, while others may experience gradual symptom return over extended periods. This variation underscores the importance of discussing individual prognosis with your treating physician.
Can I stop HBOT treatment early?
While patients can technically discontinue treatment at any time, doing so before completing the prescribed protocol typically results in substantially diminished and less durable benefits. Completing the full treatment course significantly improves the likelihood of achieving lasting therapeutic improvement. Discussing any concerns about treatment protocol with your physician is important before making modifications.
How often should I have maintenance HBOT?
Maintenance frequency depends entirely on individual circumstances and the condition being treated. Some patients benefit from occasional sessions, while others require no maintenance therapy whatsoever. Your HBOT physician can recommend appropriate maintenance protocols based on your specific situation and treatment response.
What conditions show the longest-lasting HBOT benefits?
Acute conditions like decompression sickness and carbon monoxide poisoning typically show permanent resolution. Chronic wounds often maintain improvement for 6-12 months or longer. Radiation injury treatment frequently produces benefits persisting for years or decades. Neurological conditions show more variable durability.
Can lifestyle changes extend HBOT benefits?
Absolutely. Smoking cessation, excellent diabetes control, proper nutrition, and infection prevention all substantially enhance HBOT effectiveness and extend the duration of therapeutic benefits. Addressing modifiable risk factors throughout and after treatment maximizes your investment in HBOT.
Is HBOT permanent?
For some conditions, HBOT produces permanent improvement. For others, benefits gradually diminish over time. The permanence depends on whether HBOT has achieved complete tissue repair or merely improved the condition. Your physician can discuss the expected permanence for your specific situation.



