
How Mindfulness Aids Gingival Health: Expert Insights
Gingival recession, the progressive loss of gum tissue that exposes tooth roots, affects millions worldwide and significantly impacts oral health and aesthetic appearance. While traditional dental interventions remain essential, emerging research reveals that mindfulness practices offer powerful supportive therapy for gingival recession by reducing stress-induced inflammation, improving oral hygiene habits, and promoting tissue healing. This comprehensive exploration examines the scientific mechanisms connecting mindfulness to gingival health and provides practical strategies for integrating contemplative practices into your oral care routine.
The relationship between mental wellness and oral health has long been established in medical literature, yet many patients overlook the psychological dimension of gingival disease. Stress activates the hypothalamic-pituitary-adrenal (HPA) axis, triggering cortisol release and systemic inflammation that directly compromises gum tissue integrity. Mindfulness-based interventions interrupt this cascade by modulating the nervous system, reducing inflammatory markers, and fostering behavioral changes that protect periodontal tissues. Understanding this mind-body connection empowers patients to take proactive steps in managing gingival health beyond conventional brushing and flossing.
Understanding Gingival Recession and Its Causes
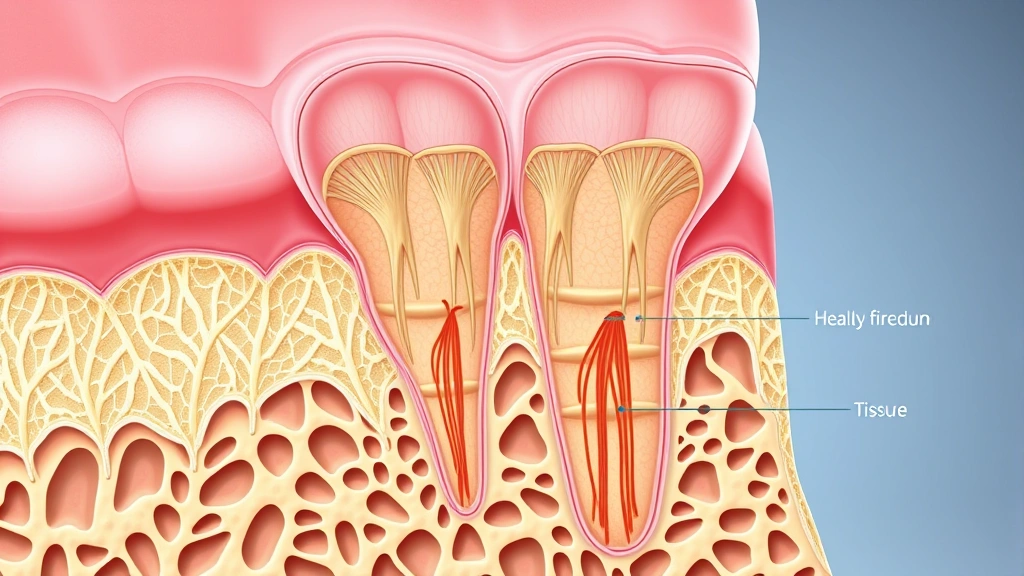
Gingival recession occurs when the gum margin moves apically, exposing the root surface and creating periodontal pockets susceptible to bacterial colonization. The condition develops through multifactorial mechanisms including aggressive tooth brushing, periodontal disease, genetic predisposition, hormonal fluctuations, and chronic psychological stress. Patients experiencing gingival recession often report heightened anxiety about their appearance and fear regarding tooth loss, creating a vicious cycle where psychological distress exacerbates the underlying condition.
The pathophysiology of gingival recession involves breakdown of collagen and proteoglycan in the extracellular matrix, coupled with reduced fibroblast activity and impaired wound healing responses. Traditional interventions focus on mechanical plaque removal, antimicrobial therapy, and surgical grafting procedures. However, these approaches address only the symptomatic manifestations while neglecting the systemic factors that perpetuate tissue degradation. Incorporating therapy resources and articles from MindLift Daily about stress management provides patients with holistic treatment frameworks that complement conventional dental care.
Research published in the Journal of Periodontology demonstrates that patients with untreated stress and anxiety exhibit significantly greater gingival recession progression and poorer response to conventional periodontal therapy. This evidence underscores the necessity of addressing psychological dimensions as integral components of comprehensive gingival health management.

The Stress-Inflammation Connection in Periodontal Disease
Chronic stress fundamentally alters immune function through multiple pathways, creating an inflammatory microenvironment that damages periodontal tissues. When individuals experience sustained psychological pressure, the sympathetic nervous system remains hyperactivated, maintaining elevated cortisol levels that suppress protective immune responses while amplifying pro-inflammatory cytokine production. This paradoxical immunosuppression increases susceptibility to pathogenic bacteria while simultaneously promoting destructive inflammation.
The hypothalamic-pituitary-adrenal axis dysfunction observed in chronically stressed individuals directly impairs the gingival epithelial barrier function. Studies from National Center for Biotechnology Information reveal that psychological stress significantly increases interleukin-6 and tumor necrosis factor-alpha levels in gingival crevicular fluid, markers strongly associated with periodontal destruction. Additionally, stress-induced behavioral changes—including reduced oral hygiene compliance, increased grinding and clenching, and dietary modifications—create mechanical and chemical conditions favorable to gingival recession.
The bidirectional relationship between stress and periodontal disease creates clinical challenges, as gingival recession itself generates anxiety and social distress, perpetuating the inflammatory cycle. Breaking this pattern requires interventions targeting both the psychological stressor and its physiological consequences. Mindfulness-based approaches uniquely address this bidirectional relationship by simultaneously reducing stress perception and promoting parasympathetic nervous system activation.
Mindfulness Mechanisms for Gum Tissue Health
Mindfulness practice—defined as non-judgmental present-moment awareness—activates the parasympathetic nervous system and downregulates the stress response cascade. Neuroimaging studies demonstrate that regular meditation increases gray matter density in the prefrontal cortex and anterior cingulate cortex, brain regions responsible for emotion regulation and stress buffering. These neuroplastic changes translate into reduced cortisol secretion, decreased inflammatory cytokine production, and enhanced immune regulation—all factors critical for gingival tissue integrity.
The mechanisms through which mindfulness supports gingival health operate across multiple biological systems. First, mindfulness reduces cortisol and catecholamine levels, thereby decreasing systemic inflammation and improving immune surveillance of pathogenic bacteria. Second, mindfulness enhances parasympathetic tone, promoting tissue repair mechanisms and collagen synthesis essential for maintaining gingival architecture. Third, mindfulness cultivation improves interoceptive awareness, enabling individuals to recognize early signs of gingival inflammation and respond proactively with enhanced oral hygiene practices.
Furthermore, mindfulness practice reduces rumination and catastrophic thinking patterns that amplify stress responses. Patients with gingival recession frequently experience intrusive thoughts about their condition, generating anxiety that perpetuates the physiological stress response. Mindfulness training interrupts this cognitive pattern by developing metacognitive awareness—the ability to observe thoughts without identification or emotional reactivity. This psychological distance from anxious thoughts reduces the emotional amplification of stress and prevents the sustained HPA axis activation that damages periodontal tissues. Research examining insurance coverage for therapy approaches indicates increasing recognition of mindfulness interventions as legitimate therapeutic modalities worthy of clinical support.
Evidence-Based Mindfulness Practices for Gingival Health
Mindfulness-based stress reduction (MBSR) programs, originally developed by Jon Kabat-Zinn at the University of Massachusetts Medical School, have demonstrated efficacy in reducing periodontal inflammation markers. An eight-week MBSR curriculum typically includes daily meditation practice, body scan exercises, mindful movement, and informal mindfulness integration into daily activities. Clinical trials examining MBSR effects on periodontal health reveal significant reductions in bleeding on probing, probing depths, and gingival recession progression compared to control groups.
Specific mindfulness techniques particularly beneficial for gingival health include:
- Breath-focused meditation: Diaphragmatic breathing activates the vagus nerve, promoting parasympathetic dominance and reducing inflammatory signaling. Ten to fifteen minutes daily produces measurable reductions in stress hormones.
- Body scan meditation: Systematically directing attention through body regions enhances interoceptive awareness, enabling individuals to recognize tension patterns affecting jaw clenching and bruxism—mechanical factors contributing to gingival recession.
- Loving-kindness meditation: Cultivating compassion toward oneself and others reduces self-critical rumination and promotes psychological resilience, buffering against stress-induced inflammation.
- Mindful eating: Conscious awareness during meals improves nutritional choices, supporting adequate intake of collagen-promoting vitamin C and bone-supporting minerals essential for periodontal health.
- Mindful oral hygiene: Bringing full attention to brushing and flossing practices increases mechanical efficacy while creating a grounding ritual that interrupts stress-reactive patterns.
Research from American Psychological Association documents that consistent mindfulness practice produces measurable changes in immune function within 8-12 weeks, with benefits increasing substantially over 6-12 months of sustained practice. The dose-response relationship suggests that daily practice exceeding 20 minutes produces optimal outcomes for periodontal health.
Integrating Mindfulness with Professional Dental Care
Optimal gingival health requires integrated treatment combining professional dental interventions with mindfulness-based supportive therapy. Patients should work collaboratively with both dental and mental health professionals to develop comprehensive treatment plans addressing mechanical, microbial, and psychological dimensions of gingival disease. Dental professionals increasingly recognize that patient motivation and compliance significantly influence treatment outcomes, and mindfulness practices enhance these behavioral factors.
The integration process begins with thorough psychological assessment to identify stress levels, anxiety patterns, and coping mechanisms relevant to gingival health. Patients demonstrating elevated stress or anxiety benefit from concurrent participation in mindfulness-based interventions, either through formal MBSR programs or guided practice with experienced teachers. Many dental offices now incorporate mindfulness elements into patient education, teaching techniques for managing dental anxiety and promoting oral hygiene compliance.
Professional periodontal treatment—including scaling and root planing, antimicrobial therapy, and in severe cases surgical intervention—remains essential for managing active periodontal disease. Mindfulness practices enhance treatment efficacy by reducing post-treatment inflammation, improving wound healing responses, and promoting behavioral adherence to maintenance protocols. Patients receiving combined conventional and mindfulness-based care demonstrate superior long-term outcomes compared to those receiving conventional treatment alone.
For individuals considering physical therapy for associated musculoskeletal conditions, mindfulness integration addresses the psychosomatic dimensions of tension-related gingival disease. Temporomandibular joint dysfunction and muscle tension patterns frequently accompany gingival recession, and mindfulness-based approaches effectively reduce these comorbid conditions.
Practical Daily Mindfulness Routines
Implementing mindfulness practice requires establishing sustainable daily routines that fit individual lifestyles and preferences. Begin with modest commitments—even five minutes daily produces measurable benefits—gradually expanding practice duration as comfort increases. The following structured approach provides a practical framework for integrating mindfulness into daily life for gingival health support:
- Morning meditation (10 minutes): Upon waking, before checking devices, sit comfortably and focus attention on natural breathing. When attention wanders—inevitable and non-problematic—gently redirect focus to breath sensations. This establishes parasympathetic dominance throughout the day.
- Mindful oral hygiene (3-5 minutes): During morning and evening brushing, bring complete attention to sensations: bristle texture, mint flavor, water temperature, gum sensations. Avoid multitasking or rumination during this grounding practice.
- Midday breathing break (3 minutes): Pause during work or daily activities for three conscious breathing cycles, creating stress-interrupting moments that prevent cortisol accumulation.
- Body scan meditation (15 minutes, 3-4 times weekly): Lie comfortably and systematically direct attention through body regions, noticing tension patterns without attempting change. This practice reveals stress-induced jaw clenching and tension patterns.
- Evening loving-kindness practice (10 minutes): Cultivate compassion by directing phrases of goodwill toward yourself, loved ones, neutral individuals, and challenging people. This reduces rumination and promotes emotional regulation.
- Mindful eating (at least one meal daily): Consume meals without distractions, noticing flavors, textures, and satiety signals. Choose nutrient-dense foods supporting periodontal health: leafy greens, fatty fish, berries, nuts.
Consistency matters more than duration; daily practice of modest length produces superior outcomes compared to occasional longer sessions. Many individuals benefit from app-based guided practices, meditation groups, or formal MBSR courses providing structure and community support. The investment in mindfulness practice yields compound benefits extending beyond gingival health to overall wellness, stress resilience, and quality of life.
Research examining occupational therapy approaches demonstrates that integrated wellness interventions produce superior health outcomes. Similarly, occupational therapists increasingly incorporate mindfulness into comprehensive health programs, recognizing its role in preventing and managing chronic conditions including periodontal disease.
FAQ
Can mindfulness alone reverse gingival recession?
Mindfulness functions as supportive therapy that enhances the body’s natural healing capacity and reduces inflammatory factors perpetuating gingival recession. However, significant recession typically requires professional dental intervention including scaling, root planing, or surgical grafting. Mindfulness optimizes treatment outcomes and prevents further recession progression by addressing underlying stress-inflammation mechanisms.
How long before mindfulness practice produces measurable gingival health improvements?
Physiological changes including reduced inflammatory markers occur within 2-4 weeks of consistent daily practice. Clinically observable improvements in gingival health typically manifest within 8-12 weeks, with continued progression through 6-12 months. Individual variation exists based on practice consistency, baseline stress levels, and concurrent dental treatment.
What mindfulness approach works best for gingival health?
Research indicates that combined approaches prove most effective: daily breath meditation (10-15 minutes) for stress reduction, body scan practice (15 minutes, 3-4 times weekly) for tension pattern awareness, and mindful oral hygiene routines for behavioral integration. Formal MBSR programs provide structured learning and community support, though individual practice with quality guidance also produces excellent outcomes.
Can mindfulness reduce dental anxiety affecting gingival health?
Yes, mindfulness directly reduces dental anxiety through multiple mechanisms: parasympathetic activation decreases fear responses, present-moment focus interrupts catastrophic thinking, and regular practice builds emotional resilience. Patients practicing mindfulness report significantly lower anxiety during dental procedures and improved treatment compliance.
Should mindfulness replace conventional dental treatment?
Absolutely not. Mindfulness serves as complementary supportive therapy enhancing conventional treatment outcomes, not replacement. Professional periodontal care remains essential for managing active disease. The optimal approach combines evidence-based dental intervention with mindfulness-based stress reduction for comprehensive gingival health management.
Are there contraindications to mindfulness practice for periodontal patients?
Mindfulness practice is generally safe for all individuals. However, those with significant trauma histories or certain psychiatric conditions may benefit from guidance from trained professionals. Mental health providers can help individuals adapt practices to their specific needs and integrate mindfulness safely with existing treatments.


