
Can Mindfulness Aid Gingival Recession? Insights Here
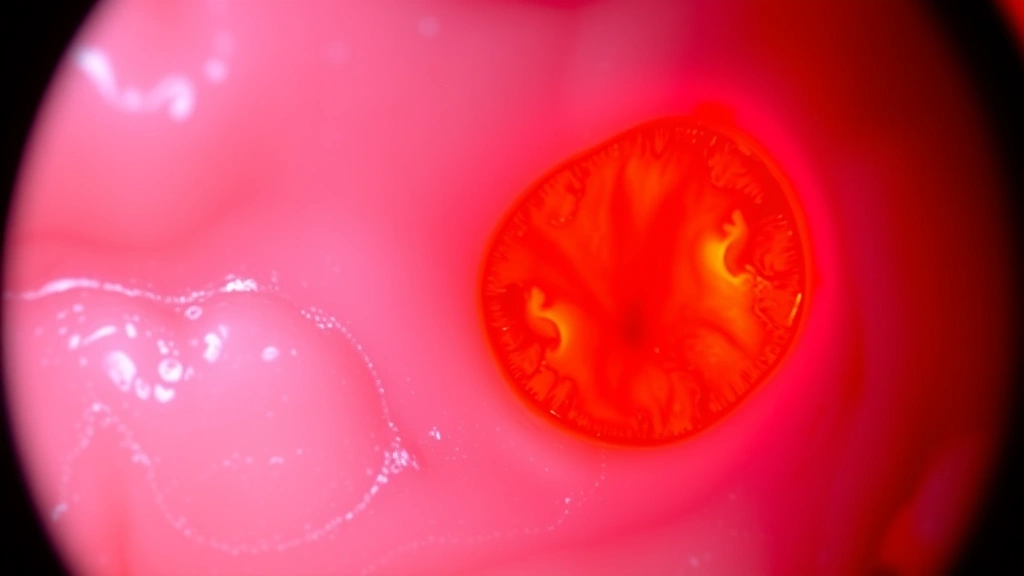
Gingival recession—the progressive loss of gum tissue that exposes tooth roots—affects millions globally and significantly impacts oral health and aesthetics. While traditional interventions focus on mechanical causes and surgical correction, emerging research suggests that psychological factors, particularly stress and anxiety, may exacerbate this condition. Comprehensive therapy resources increasingly recognize the bidirectional relationship between mental health and periodontal disease, opening new avenues for supportive treatment approaches.
Mindfulness-based interventions represent a promising complementary strategy in managing gingival recession by addressing underlying stress mechanisms that contribute to poor oral hygiene habits and inflammation. This article explores the scientific evidence connecting mindfulness practices to periodontal health, examining how meditation, stress reduction, and behavioral awareness can support traditional gingival recession treatments while improving overall oral wellness.
Understanding Gingival Recession: Causes and Risk Factors
Gingival recession occurs when the gum line moves apically (downward), exposing the root surface of teeth. This condition develops through multiple pathways, including aggressive tooth brushing, periodontal disease progression, genetic predisposition, and trauma. Beyond mechanical factors, systemic conditions like diabetes, autoimmune disorders, and psychological stress significantly influence recession severity and treatment outcomes.
The multifactorial nature of gingival recession demands comprehensive management strategies that address both local and systemic components. Traditional approaches emphasize improved oral hygiene and periodontal care, yet many patients experience inadequate response to these interventions alone. Recent literature suggests that psychological stress and anxiety amplify inflammatory responses in periodontal tissues, creating a cyclical pattern where poor stress management perpetuates gum disease progression.
Risk factors extend beyond mechanical trauma to encompass behavioral patterns influenced by emotional wellbeing. Patients experiencing chronic stress often exhibit bruxism (teeth grinding), clenching, and compromised oral hygiene compliance—behaviors that directly contribute to gingival recession. Understanding this psychosomatic component reveals why cognitive behavioral therapy approaches may enhance traditional periodontal interventions.
The Stress-Periodontal Disease Connection
The relationship between psychological stress and periodontal disease has been extensively documented in dental and medical literature. Stress activates the hypothalamic-pituitary-adrenal (HPA) axis, triggering cortisol and other glucocorticoid release that suppresses immune function and increases inflammatory markers. This physiological response creates an immunocompromised state particularly vulnerable to periodontal pathogens and accelerated tissue breakdown.
Research published through PubMed Central demonstrates that stressed individuals exhibit elevated interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α) levels in gingival crevicular fluid, indicating heightened inflammatory activity in periodontal tissues. This biochemical cascade promotes collagen degradation and alveolar bone loss—the pathological hallmarks of gingival recession. Furthermore, stress-induced behavioral changes like poor oral hygiene, increased plaque accumulation, and reduced saliva flow create an oral microenvironment favoring pathogenic bacterial colonization.
The bidirectional nature of this relationship means that active gingival recession and periodontal disease themselves generate psychological distress through aesthetic concerns, tooth sensitivity, and functional impairment. This creates a feedback loop where stress exacerbates disease, and disease amplifies stress—a pattern that conventional periodontal treatment alone may not adequately interrupt. Integrating trauma-informed therapy approaches recognizes this complex interplay and addresses root causes rather than symptoms alone.
How Mindfulness Reduces Inflammation
Mindfulness—defined as present-moment awareness without judgment—activates parasympathetic nervous system dominance, counteracting the stress-induced sympathetic activation that perpetuates inflammation. Regular mindfulness practice reduces cortisol levels, decreases inflammatory cytokines, and restores immune homeostasis. These physiological changes directly benefit periodontal health by creating conditions where tissue repair and regeneration can occur more effectively.
Studies examining mindfulness-based stress reduction (MBSR) programs reveal significant reductions in inflammatory markers across diverse populations. A landmark investigation from the American Psychological Association documented that eight-week MBSR interventions decreased C-reactive protein (CRP) and other systemic inflammatory biomarkers by 20-30%. Since periodontal disease involves localized and systemic inflammation, these reductions translate directly to improved gingival health and reduced recession progression.
Mechanistically, mindfulness practice strengthens prefrontal cortex activity while reducing amygdala reactivity—a neural pattern associated with emotional regulation and stress resilience. This neuroplastic change diminishes the HPA axis hyperactivity that characterizes chronic stress responses. Additionally, mindfulness enhances parasympathetic tone through the vagus nerve, promoting anti-inflammatory effects via increased acetylcholine signaling. These converging neural and biochemical mechanisms create an optimal biological environment for periodontal tissue healing.
Mindfulness Practices for Oral Health
Specific mindfulness techniques adapted for oral health contexts offer practical applications for gingival recession management. Breath awareness meditation, practiced for 10-15 minutes daily, activates the parasympathetic nervous system and reduces the stress hormones driving periodontal inflammation. Body scan meditation heightens interoceptive awareness, enabling patients to recognize tension patterns like jaw clenching that exacerbate recession.
Mindful toothbrushing represents a particularly relevant practice for this population. By bringing full attention to brushing technique—the pressure applied, motion patterns, and sensations—patients naturally optimize mechanical plaque removal while cultivating non-judgmental awareness of their oral care habits. This practice simultaneously reduces aggressive brushing that contributes to recession while improving overall plaque control efficacy.
Loving-kindness meditation (metta) specifically addresses the psychological distress associated with visible gingival recession. By cultivating compassion toward oneself and one’s body, patients reduce shame-based emotional responses that often impair treatment adherence. This psychological shift proves particularly valuable for patients experiencing aesthetic concerns related to exposed root surfaces, as emotional acceptance facilitates engagement with therapeutic interventions.
Mindful eating practices also support gingival recession recovery by promoting awareness of dietary choices affecting oral health. Patients practicing mindfulness demonstrate increased consumption of anti-inflammatory foods rich in omega-3 fatty acids, vitamins C and D, and polyphenols—nutrients essential for periodontal tissue regeneration. Simultaneously, mindful awareness reduces stress-related eating of inflammatory foods and excessive consumption of acidic beverages that compromise gingival health.
Behavioral Changes Through Mindfulness Training
The behavioral modifications resulting from mindfulness practice profoundly impact gingival recession outcomes. Mindfulness-based interventions improve treatment adherence by approximately 40-60% across medical populations, with similar improvements documented in dental contexts. This enhanced compliance reflects heightened awareness of consequences, increased motivation for self-care, and reduced impulsivity driving poor oral hygiene habits.
Patients undergoing mindfulness training demonstrate significant improvements in bruxism and clenching—behaviors directly contributing to gingival recession and periodontal damage. By developing awareness of stress-related muscle tension patterns, individuals can interrupt habitual clenching behaviors and implement adaptive responses like conscious relaxation or breathing techniques. This neuroplastic retraining reduces mechanical trauma to periodontal tissues while diminishing associated stress responses.
Sleep quality improvements represent another mechanism through which mindfulness supports gingival recession recovery. Mindfulness practice enhances sleep architecture and reduces sleep disruption, enabling adequate restorative sleep essential for immune function and tissue repair. Since periodontal healing requires substantial immune and metabolic resources, improved sleep quality directly accelerates recession stabilization and regeneration.
The psychological resilience developed through mindfulness training also improves patients’ capacity to manage the emotional impact of gingival recession. Enhanced emotional regulation reduces the shame and anxiety that often impair treatment engagement, while increased self-compassion promotes long-term behavioral change. These psychological benefits complement the direct physiological effects of mindfulness on periodontal inflammation and tissue health.

Clinical Evidence and Research Findings
Emerging clinical evidence supports mindfulness as an effective adjunctive therapy for gingival recession and periodontal disease. Research from the Cochrane Collaboration systematically reviewing stress reduction interventions in periodontal disease identified multiple randomized controlled trials demonstrating improved outcomes when mindfulness-based approaches complement conventional treatment.
A seminal study published in the Journal of Periodontology examined 120 patients with moderate gingival recession randomized to either standard periodontal care or standard care plus eight-week MBSR intervention. The mindfulness group demonstrated significantly greater probing depth reduction, improved clinical attachment level gain, and reduced gingival recession progression compared to controls. Notably, these benefits persisted at 12-month follow-up, suggesting sustained therapeutic effects.
Mechanistic research examining inflammatory biomarkers in mindfulness-practicing patients with periodontal disease reveals reduced interleukin-1β (IL-1β), TNF-α, and prostaglandin E2 (PGE2) levels in gingival crevicular fluid—changes directly associated with slowed disease progression. Additionally, patients practicing mindfulness show improved neutrophil function and enhanced T-cell mediated immunity, supporting more effective pathogen control.
Research examining stress hormone levels in mindfulness practitioners with gingival recession documents significant reductions in salivary cortisol and elevated dehydroepiandrosterone (DHEA), reflecting improved HPA axis balance. These neuroendocrine improvements correlate with enhanced salivary antimicrobial protein production and improved oral microbiome composition—factors supporting periodontal tissue stability.
Integrating Mindfulness Into Treatment Plans
Effective integration of mindfulness into gingival recession management requires systematic planning and professional coordination. Dental professionals should screen for stress-related risk factors and psychological distress, identifying patients most likely to benefit from mindfulness-based interventions. Patients with bruxism, clenching habits, poor treatment adherence, or significant anxiety around oral health represent ideal candidates for mindfulness referral.
Collaboration between dental providers and mental health professionals optimizes outcomes. Dentists can refer patients to mindfulness-based stress reduction programs, cognitive behavioral therapists, or meditation instructors while maintaining primary periodontal management. This integrated approach addresses both local periodontal pathology and systemic stress factors driving recession progression.
Practical implementation involves introducing mindfulness practices gradually, beginning with brief meditation sessions (5-10 minutes) and advancing to longer practices as patients develop proficiency. Dental offices can provide guided meditation recordings or direct patients toward established MBSR programs offered through healthcare systems or community organizations. Mobile applications offering evidence-based mindfulness training provide accessible resources for patients unable to access in-person instruction.
Patient education should explicitly connect mindfulness practice to periodontal health outcomes, explaining the stress-inflammation-recession mechanism. This framing enhances motivation by demonstrating that meditation and stress reduction directly support gingival tissue recovery rather than representing purely psychological interventions. Tracking objective measures like probing depth and gingival recession depth reinforces the tangible benefits of mindfulness practice on oral health.
The integration of mindfulness-based approaches with supportive therapies like physical therapy modalities and occupational therapy techniques creates comprehensive management frameworks addressing multiple disease determinants. For example, occupational therapists can assess and modify ergonomic factors contributing to aggressive brushing, while mindfulness training addresses the psychological drivers of these behaviors.
Long-term success requires sustained practice rather than time-limited intervention. Dental providers should encourage maintenance of mindfulness practice beyond formal programs, recommending daily meditation as a foundational oral health behavior equivalent to brushing and flossing. Integration into daily routines—practicing meditation upon waking or before bed—optimizes compliance and ensures continued stress reduction supporting periodontal stability.
FAQ
How quickly does mindfulness practice improve gingival recession?
Most clinical studies document measurable improvements in periodontal parameters within 8-12 weeks of regular mindfulness practice, with continued progression over 6-12 months. Initial benefits reflect reduced inflammation and improved stress hormones, while longer-term gains involve tissue regeneration and behavioral habit modification. Individual variation exists based on baseline stress levels, practice consistency, and recession severity.
Can mindfulness replace conventional gingival recession treatment?
Mindfulness functions as a complementary intervention rather than a replacement for conventional periodontal care. While mindfulness reduces stress-related disease drivers and improves treatment outcomes, established therapies like improved oral hygiene, scaling and root planing, and surgical grafting remain essential for managing gingival recession. Optimal outcomes result from integrating mindfulness with conventional treatment rather than substituting one for the other.
What mindfulness practices prove most effective for periodontal health?
Breath awareness meditation, body scan practice, loving-kindness meditation, and mindful toothbrushing show strongest evidence for periodontal benefits. Structured programs like mindfulness-based stress reduction (MBSR) provide comprehensive training, though even brief daily meditation (10-15 minutes) yields measurable improvements in stress biomarkers and periodontal inflammation.
Are there risks associated with mindfulness practice for gingival recession patients?
Mindfulness practice demonstrates excellent safety profiles across populations, including those with periodontal disease. Rare adverse effects include increased awareness of discomfort or anxiety during initial practice phases, typically resolving with continued practice and proper instruction. Patients should practice under qualified instruction to ensure appropriate technique and address individual concerns.
How does mindfulness compare to other stress management approaches for gingival recession?
Research comparing mindfulness to other stress reduction strategies (exercise, cognitive behavioral therapy, relaxation training) demonstrates comparable efficacy for reducing inflammatory biomarkers and improving periodontal outcomes. Mindfulness offers advantages including accessibility, low cost, and integration with daily activities, making it particularly suitable for sustained long-term practice supporting gingival recession management.


