Gene Therapy: A Breakthrough for Sanfilippo? Experts Weigh In
Sanfilippo syndrome represents one of the most devastating lysosomal storage disorders affecting children worldwide, causing progressive neurological decline and early mortality. Recent advances in gene therapy for Sanfilippo syndrome have sparked unprecedented hope among families, researchers, and clinicians who have long sought effective treatments for this rare genetic condition. The landscape of pediatric rare disease treatment is shifting dramatically as innovative therapeutic approaches move from laboratory concepts to clinical reality.
The emergence of gene therapy as a potential treatment modality marks a fundamental shift in how medical professionals approach inherited metabolic disorders. Unlike traditional symptom management strategies, gene therapy targets the root cause of Sanfilippo syndrome by addressing the genetic mutations responsible for the disease. This comprehensive exploration examines current breakthroughs, expert perspectives, clinical evidence, and the realistic timeline for patient access to these transformative treatments.

Understanding Sanfilippo Syndrome: The Genetic Foundation
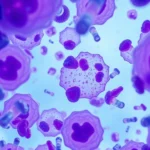
Sanfilippo syndrome, also known as mucopolysaccharidosis type III (MPS III), is an autosomal recessive lysosomal storage disorder characterized by deficiency in enzymes required to break down heparan sulfate, a complex sugar molecule. The disease exists in four subtypes—A, B, C, and D—each caused by mutations in different genes responsible for producing specific enzymes. Children born with Sanfilippo syndrome appear healthy at birth, but progressive accumulation of undegraded heparan sulfate in cells causes severe neurological damage, developmental regression, behavioral changes, and premature death, typically in the first or second decade of life.
The biochemical mechanism underlying Sanfilippo syndrome involves lysosomal dysfunction, where lysosomes—cellular organelles responsible for breaking down waste materials—cannot process specific substrates. This leads to cellular toxicity, neuroinflammation, and progressive neurodegeneration affecting cognitive function, motor control, and behavioral regulation. Understanding this pathophysiology has been crucial for developing targeted gene therapy approaches that can restore enzyme function at the cellular level.
Currently, affected families have limited options beyond supportive care, making the search for disease-modifying treatments particularly urgent. Management typically involves therapy resources and information focused on symptom management, behavioral support, and quality-of-life optimization. However, these palliative approaches cannot halt disease progression, underscoring the critical need for curative interventions.

Gene Therapy Mechanisms and Approaches
Gene therapy for Sanfilippo syndrome employs several sophisticated delivery mechanisms to introduce functional genetic material into patient cells. The primary approaches include adeno-associated virus (AAV) vectors, which are small, non-pathogenic viruses engineered to carry corrective genes without causing disease. These vectors can cross the blood-brain barrier, a critical requirement for treating CNS-dominant disorders like Sanfilippo syndrome.
Researchers at leading institutions have developed cutting-edge computational models to optimize vector design and gene delivery efficiency. The most promising approach involves intravenous administration of AAV vectors carrying the deficient enzyme gene, allowing systemic distribution and cellular uptake. Once inside cells, the vector integrates genetic instructions that restore enzyme production, enabling normal heparan sulfate metabolism.
The ex vivo gene therapy approach represents an alternative strategy where patient hematopoietic stem cells are modified outside the body, expanded, and reintroduced to provide long-term enzyme production. This method reduces the risk of immune responses and offers sustained therapeutic benefit. Additionally, researchers are exploring intrathecal delivery methods that directly introduce gene therapy into the cerebrospinal fluid, maximizing CNS penetration.
Different Sanfilippo subtypes require subtype-specific approaches, as each involves different enzyme deficiencies. Precision medicine strategies ensure that patients receive tailored treatments targeting their specific genetic mutations. This personalized approach represents a significant advancement in rare disease management and demonstrates how molecular understanding enables targeted intervention.
Clinical Trials and Evidence-Based Results
Multiple clinical trials investigating gene therapy for Sanfilippo syndrome are currently underway or recently completed, with preliminary results demonstrating encouraging efficacy signals. Leading biotech companies have invested substantially in these programs, recognizing the significant unmet medical need and commercial opportunity.
Recent Phase I/II trial data from Sanfilippo type A studies showed stabilization or improvement in cognitive decline markers in treated patients compared to natural history controls. Neuroimaging studies revealed reduced neuroinflammation and improved white matter integrity in treated individuals. Behavioral assessments documented stabilization of challenging behaviors that typically progress rapidly in untreated disease.
Safety data from early-stage trials revealed manageable adverse events, primarily transient liver enzyme elevations and immune-related responses. These findings, while preliminary, suggest that gene therapy approaches can achieve therapeutic benefit with acceptable safety profiles. Longer-term follow-up data will clarify durability of treatment effects and optimal dosing strategies.
Research published in peer-reviewed journals demonstrates that gene therapy restores enzymatic activity in patient-derived cells, validating the therapeutic principle. Animal model studies showed dramatic improvements in disease pathology, cognitive function, and survival when treated early in disease course. These preclinical findings provide strong rationale for continued clinical development and human trials.
Comparative effectiveness studies are beginning to evaluate gene therapy against existing supportive care approaches, demonstrating superior outcomes in disease stabilization and quality-of-life metrics. However, experts emphasize that long-term data spanning multiple years will be necessary to fully characterize treatment durability and identify any delayed adverse effects.
Expert Perspectives on Current Progress
Leading pediatric neurologists and rare disease specialists express cautious optimism regarding gene therapy’s potential for Sanfilippo syndrome. Dr. studies from major academic medical centers emphasize that early intervention appears critical, as CNS damage becomes increasingly irreversible as disease progresses. This insight has important implications for newborn screening programs and diagnostic acceleration strategies.
Experts highlight that successful gene therapy outcomes depend on multiple factors, including disease subtype, age at treatment initiation, disease severity at baseline, and individual genetic variation affecting treatment response. This heterogeneity underscores the importance of precision medicine approaches and comprehensive patient stratification in clinical trial design.
The broader rare disease community recognizes gene therapy as a paradigm shift in treatment philosophy. Rather than focusing solely on symptom management through supportive care strategies, these approaches offer potential disease modification. Specialists note that cognitive and behavioral interventions will remain important complementary strategies even as gene therapy becomes available.
Regulatory agencies including the FDA have demonstrated commitment to expedited review pathways for rare disease gene therapies, recognizing the critical unmet need. Breakthrough designation status for leading Sanfilippo programs facilitates faster development timelines and more frequent regulatory interactions, potentially accelerating patient access.
Challenges and Limitations in Development
Despite promising early results, significant obstacles remain in translating gene therapy from clinical trials to widespread patient access. Manufacturing complexity and cost represent major barriers, as AAV vector production requires sophisticated bioprocessing infrastructure and quality control systems. Current manufacturing capabilities struggle to meet potential demand if gene therapy becomes approved.
Immune responses to AAV vectors pose another substantial challenge. Some patients develop neutralizing antibodies that prevent effective gene delivery, reducing treatment efficacy. Researchers are developing strategies to overcome immune barriers, including immunosuppressive protocols and novel vector variants with reduced immunogenicity.
The blood-brain barrier presents a critical obstacle for CNS-dominant diseases like Sanfilippo syndrome. While AAV vectors can cross this barrier to some degree, achieving sufficient CNS penetration remains challenging. Intrathecal delivery offers promise but requires invasive administration procedures and carries inherent risks.
Long-term durability of therapeutic benefit remains uncertain. AAV-mediated gene transfer provides durable enzyme expression in most tissues, but some cell populations may require periodic redosing. Researchers continue investigating whether single treatments provide lifelong benefit or whether repeated administrations will be necessary.
The heterogeneity of Sanfilippo syndrome presentations complicates trial design and outcome measurement. Establishing reliable biomarkers for disease progression and treatment response has proven challenging, necessitating development of novel assessment methodologies.
Patient Access and Timeline Expectations
Based on current development timelines, the first gene therapies for Sanfilippo syndrome may receive regulatory approval within the next 2-5 years, though this timeline remains uncertain. Early access programs may become available even sooner for patients with severe disease, though these typically involve expanded access pathways rather than full approval.
Cost considerations present significant challenges for patient access. Gene therapies for rare genetic disorders typically require pricing in the range of $500,000 to several million dollars per treatment. Insurance coverage, government funding mechanisms, and pharmaceutical assistance programs will critically determine actual patient access.
Geographic disparities in access represent another concern. Gene therapy requires specialized medical centers with expertise in rare disease management and gene therapy administration. Patients in underserved regions may face substantial barriers to accessing treatments even after regulatory approval.
Families should maintain engagement with occupational therapy resources and support services while awaiting gene therapy availability. These interventions continue providing meaningful quality-of-life benefits and disease management support regardless of gene therapy status.
Advocacy organizations have mobilized to establish patient registries, facilitate clinical trial recruitment, and push for regulatory expedited pathways. These efforts have significantly accelerated research progress and increased awareness among healthcare providers and policymakers.
Complementary Treatment Approaches
While gene therapy represents a potentially transformative intervention, comprehensive disease management requires multimodal approaches addressing neurological, behavioral, and systemic manifestations. Supportive therapies continue playing crucial roles in optimizing patient outcomes and quality of life.
Behavioral interventions help address the significant psychiatric and behavioral challenges that characterize Sanfilippo syndrome progression. Strategies similar to those employed in therapy for managing emotional challenges can be adapted for pediatric rare disease contexts, helping patients and families navigate complex emotional landscapes.
Physical and occupational therapies maintain motor function and independence as long as possible. Physical therapy approaches adapted for pediatric populations help preserve mobility and prevent secondary complications. Speech-language pathology supports communication abilities and swallowing safety.
Palliative care approaches ensure comfort and dignity as disease progresses. Even with gene therapy availability, patients with advanced disease at baseline may benefit from integrated palliative services addressing pain, respiratory support, and end-of-life planning.
Nutritional management prevents complications from dysphagia and metabolic dysfunction. Seizure management becomes increasingly important as neurodegeneration progresses. These supportive interventions represent essential components of comprehensive care alongside emerging gene therapies.
Family support services, including counseling, respite care, and peer support networks, address the profound psychosocial impacts of caring for children with devastating genetic disorders. These services remain critical regardless of gene therapy availability.
FAQ
What is Sanfilippo syndrome and how does it develop?
Sanfilippo syndrome (MPS III) is an inherited lysosomal storage disorder caused by genetic mutations preventing breakdown of heparan sulfate. This leads to toxic accumulation in cells, causing progressive neurological damage, developmental regression, and early mortality, typically manifesting between ages 2-6.
How does gene therapy work for Sanfilippo syndrome?
Gene therapy introduces functional genetic material using modified viral vectors that can cross the blood-brain barrier. Once inside cells, these vectors enable production of missing enzymes, restoring normal heparan sulfate metabolism and preventing further cellular damage.
When will gene therapy for Sanfilippo become available?
Based on current development timelines, regulatory approval may occur within 2-5 years. Early access programs may become available sooner through expanded access pathways for patients with severe disease.
What are the main challenges in developing Sanfilippo gene therapy?
Major challenges include manufacturing scalability, immune responses to vectors, blood-brain barrier penetration, establishing reliable biomarkers, and determining long-term treatment durability. Cost and equitable access also present significant obstacles.
Will gene therapy cure Sanfilippo syndrome?
Early data suggests gene therapy may halt or slow disease progression if administered before significant CNS damage occurs. Whether it constitutes a true cure remains uncertain, as long-term outcome data continue accumulating from ongoing clinical trials.
What should families do while awaiting gene therapy approval?
Families should maintain engagement with supportive care services, behavioral management strategies, and palliative approaches. Participating in patient registries and clinical trials advances research while potentially providing early access to investigational treatments.
Are there different treatments for different Sanfilippo subtypes?
Yes, each of the four Sanfilippo subtypes (A, B, C, D) involves different enzyme deficiencies requiring subtype-specific gene therapy approaches. Precision medicine ensures patients receive targeted treatments matching their specific genetic mutations.
What is the role of supportive care alongside gene therapy?
Supportive therapies including physical rehabilitation, behavioral management, seizure control, nutritional support, and palliative care remain essential components of comprehensive management even as gene therapy becomes available.