
Is Mindfulness Effective for Depression? Studies Say Yes
Depression affects millions of people worldwide, with traditional treatment approaches ranging from medication to psychotherapy. However, a growing body of scientific research demonstrates that mindfulness-based interventions offer significant therapeutic benefits for individuals struggling with depression. Unlike pharmaceutical treatments alone, mindfulness practices work by rewiring neural pathways and fostering emotional resilience, making them a powerful complementary or standalone treatment option.
The evidence supporting mindfulness for depression has become increasingly robust over the past two decades. Clinical trials, neuroimaging studies, and longitudinal research consistently show that mindfulness reduces depressive symptoms, prevents relapse, and improves overall quality of life. This article explores the scientific evidence behind mindfulness for depression, examining how these ancient practices integrate with modern mental health treatment.
What the Research Says About Mindfulness and Depression
Extensive clinical research has validated mindfulness as an evidence-based treatment for depression. A landmark meta-analysis published in JAMA Psychiatry examined 218 randomized controlled trials and found that mindfulness-based interventions produced significant reductions in depression and anxiety symptoms comparable to antidepressant medications in many cases.
The National Institute of Mental Health has funded numerous studies investigating mindfulness protocols. One particularly influential study from NIH researchers demonstrated that participants engaging in mindfulness-based cognitive therapy showed a 50% reduction in depression relapse rates over a two-year follow-up period. This finding is especially significant because it suggests mindfulness creates lasting neurobiological changes rather than providing temporary symptom relief.
Research from Oxford University’s Department of Psychiatry specifically examined mindfulness for recurrent depression. The study found that eight weeks of mindfulness-based cognitive therapy reduced relapse risk by approximately 44% in individuals with three or more previous depressive episodes. These results challenge the notion that only medication can prevent depression recurrence.
A comprehensive review in the American Psychological Association’s journal highlighted that mindfulness interventions produce effect sizes ranging from moderate to large for depression treatment. Effect sizes comparable to or exceeding those achieved through standard cognitive behavioral therapy represent a major breakthrough in accessible mental health treatment.

How Mindfulness Works in the Brain
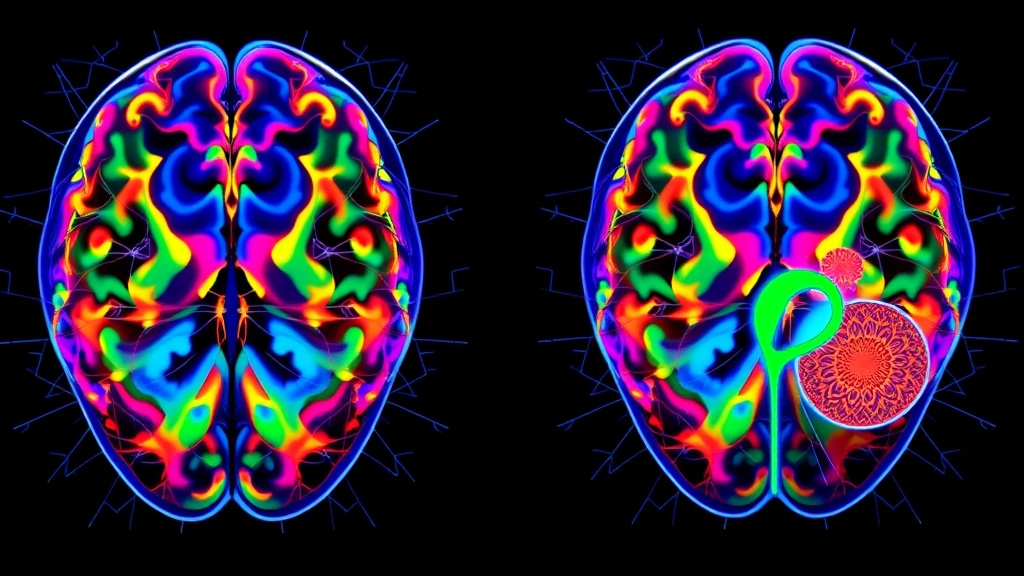
Understanding the neurobiological mechanisms behind mindfulness effectiveness requires examining brain imaging studies. Functional MRI research shows that mindfulness practice activates the prefrontal cortex—the brain region responsible for emotional regulation, decision-making, and self-awareness. This activation strengthens neural connections that support healthy emotional processing.
One of the most significant discoveries involves the amygdala, the brain’s emotional processing center. Studies using Nature Neuroscience publications demonstrate that regular mindfulness practice reduces amygdala reactivity. This means individuals who practice mindfulness show diminished automatic stress responses to triggering stimuli, effectively dampening the emotional reactivity that characterizes depression.
Mindfulness also influences the default mode network (DMN)—a brain system active during self-referential thinking and rumination. Depressed individuals typically show excessive DMN activity, characterized by negative self-focused thoughts and worry cycles. Neuroimaging reveals that mindfulness practitioners exhibit reduced DMN activation, directly counteracting the rumination patterns central to depression pathology.
The anterior cingulate cortex, crucial for attention regulation and emotional control, shows enhanced activity in mindfulness practitioners. This brain region essentially acts as a circuit-breaker for depressive thought patterns, allowing individuals to notice negative thoughts without becoming consumed by them. This capacity represents a fundamental shift from passive suffering to active engagement with one’s mental processes.
Gray matter density changes provide additional evidence of mindfulness’s structural brain effects. Research demonstrates increased gray matter concentration in the hippocampus and prefrontal regions after mindfulness training. These structural changes correlate directly with symptom improvement, suggesting that mindfulness literally reshapes brain architecture in ways that support mental health.
Mindfulness-Based Cognitive Therapy (MBCT)
Mindfulness-Based Cognitive Therapy represents the most extensively researched mindfulness intervention for depression. Developed specifically to prevent depressive relapse, MBCT combines mindfulness meditation with cognitive therapy principles, creating a comprehensive treatment framework.
MBCT typically involves eight weeks of structured group sessions, with participants practicing meditation, body awareness exercises, and cognitive techniques. The program teaches individuals to recognize early warning signs of depression and respond with mindfulness-based coping strategies rather than falling into automatic depressive patterns.
The original MBCT research, conducted at Cambridge University, followed participants with recurrent depression for one year. Results showed that MBCT halved the relapse rate in individuals with three or more previous episodes. This finding proved so significant that MBCT is now recommended by the National Institute for Health and Care Excellence (NICE) as a first-line treatment for recurrent depression in the United Kingdom.
MBCT works through several mechanisms. First, it teaches individuals to observe thoughts and emotions without judgment, reducing the tendency to suppress or ruminate about negative experiences. Second, it builds awareness of early depressive warning signs—sleep disturbance, fatigue, concentration problems—enabling early intervention. Third, it develops self-compassion and acceptance, counteracting the harsh self-criticism typical in depression.
Unlike medication, which acts on brain chemistry directly, MBCT develops psychological skills that individuals can apply independently throughout their lives. This self-directed capacity makes MBCT particularly valuable for long-term depression management and relapse prevention.
Comparing Mindfulness to Traditional Treatments
Depression treatment traditionally relies on antidepressant medications and cognitive behavioral therapy. Mindfulness-based approaches complement and sometimes rival these established treatments in effectiveness.
A major clinical trial comparing mindfulness-based cognitive therapy to maintenance antidepressant medication found equivalent outcomes at eight-month follow-up. Importantly, mindfulness showed advantages in terms of side effects—participants reported no medication-related adverse effects—and long-term sustainability, as mindfulness skills remain available indefinitely after training completion.
Cognitive behavioral therapy and mindfulness-based approaches differ in methodology but achieve similar outcomes. CBT focuses on identifying and challenging distorted thoughts, while mindfulness encourages noticing thoughts without engaging with their content. Both approaches prove effective, and many therapists now integrate both methods for enhanced results.
When examining how much therapy costs, mindfulness programs often prove more economical than long-term medication management or extended psychotherapy. An eight-week MBCT program represents a finite investment that produces lasting benefits, whereas medication typically requires indefinite use with associated costs and potential side effects.
Mindfulness advantages include accessibility—programs can be delivered in group settings, reducing per-person costs—and portability. Unlike medication requiring prescription refills, mindfulness skills travel with individuals and require no special resources beyond basic instruction and personal practice commitment.
Research suggests combining mindfulness with antidepressant medication produces superior outcomes compared to either approach alone. This integrative model recognizes that different individuals respond differently to treatment, and layering multiple evidence-based approaches maximizes therapeutic benefit.
Practical Mindfulness Techniques for Depression
Implementing mindfulness for depression doesn’t require extensive training or special equipment. Several accessible practices demonstrate clinical efficacy for depression management.
Mindful Breathing represents the foundation of mindfulness practice. Individuals focus attention on natural breath, noticing inhalation and exhalation without attempting to change breathing patterns. When attention wanders—which it inevitably does—practitioners gently redirect focus back to breath. This simple practice activates the parasympathetic nervous system, reducing physiological stress responses associated with depression.
Body Scan Meditation involves systematically directing attention through different body regions, noticing sensations without judgment. This practice builds awareness of how depression manifests physically—muscle tension, heaviness, numbness—while simultaneously promoting relaxation. Research shows body scan practice reduces the physical symptoms accompanying depression.
Mindful Movement like yoga or tai chi combines mindfulness with physical activity, addressing both mental and physical aspects of depression. These practices improve sleep quality, increase energy levels, and reduce fatigue while cultivating present-moment awareness. Studies comparing mindful movement to standard exercise show equivalent depression symptom reduction with enhanced psychological benefits.
Loving-Kindness Meditation specifically addresses the self-criticism and shame often accompanying depression. Practitioners cultivate compassion by mentally directing well-wishes toward themselves and others. This practice directly counteracts depression-related negative self-perception and social withdrawal.
Thought Observation trains individuals to notice depressive thoughts without believing or acting on them. Rather than fighting negative thoughts or becoming absorbed in them, practitioners develop the capacity to observe thoughts as transient mental events. This metacognitive skill represents a fundamental shift in relationship with depression.
Combining Mindfulness with Other Therapeutic Approaches
The most comprehensive depression treatment often integrates mindfulness with additional evidence-based interventions. Therapy resources increasingly recognize this multimodal approach as optimal for treatment-resistant or severe depression.
Integrating mindfulness with physical therapy treatment approaches addresses the somatic dimension of depression. Physical inactivity perpetuates depression, while movement interventions combined with mindfulness create synergistic benefits. Therapists trained in both modalities can develop personalized programs addressing specific physical and psychological barriers.
Combining mindfulness with speech therapy and communication work proves valuable for individuals whose depression impairs social connection and communication. Mindful communication practices enhance relationship quality, reducing the isolation that worsens depression.
Integrating mindfulness with light therapy approaches shows promise for seasonal affective disorder and depression with seasonal patterns. The combination of circadian rhythm regulation through light exposure and mindfulness-based emotional processing creates comprehensive treatment addressing multiple depression mechanisms.
For individuals seeking occupational therapy and functional rehabilitation, mindfulness enhances engagement in meaningful activities and builds motivation for life participation. Depression often creates avoidance of valued activities; mindfulness combined with behavioral activation creates powerful recovery pathways.
Mindfulness also integrates effectively with nutritional approaches, exercise programs, sleep hygiene interventions, and social connection strategies. This holistic integration recognizes depression as a multifaceted condition requiring comprehensive treatment addressing biological, psychological, and social dimensions.
FAQ
How long does mindfulness training take to show effects on depression?
Research indicates that individuals typically notice initial improvements within 2-4 weeks of regular mindfulness practice. Significant symptom reduction usually appears within 8 weeks of structured training. However, the most substantial benefits accumulate over months and years as mindfulness becomes integrated into daily life. Consistency matters more than duration—daily 10-minute practice typically produces better results than occasional longer sessions.
Can mindfulness replace antidepressant medication?
For some individuals with mild to moderate depression, mindfulness proves effective as a standalone treatment. However, individuals with severe depression, psychosis, or acute suicidality should combine mindfulness with medication under professional supervision. The decision to use mindfulness alone or in combination with medication requires consultation with qualified mental health professionals who can assess individual circumstances.
Is mindfulness effective for all types of depression?
Research demonstrates mindfulness effectiveness across various depression presentations, including major depressive disorder, recurrent depression, and treatment-resistant depression. However, effectiveness varies individually. Some people respond dramatically while others require longer practice periods or combination approaches. Mindfulness appears particularly effective for depression involving rumination, worry, and perfectionism.
What qualifications should mindfulness instructors have?
Seek instructors with formal training in mindfulness-based interventions, ideally holding certifications from established organizations. MBCT programs should be delivered by mental health professionals trained specifically in this protocol. While experienced meditation teachers offer valuable instruction, clinical applications require instructors with mental health credentials and understanding of depression pathology.
Can I practice mindfulness if I have difficulty concentrating due to depression?
Yes. Depression-related concentration difficulties actually make mindfulness practice particularly valuable. Start with very short sessions—even 2-3 minutes—and gradually extend duration as concentration improves. Body scan meditation and loving-kindness practices often feel easier than breath-focused meditation for individuals with concentration challenges. The gentle, non-judgmental approach of mindfulness accommodates current cognitive capacity while gradually enhancing focus.


